
Now that we re-oriented the structure and anatomy of the heart, let’s get into some of the basics of hemodynamics.
***students everywhere shudder****
It really won’t be that bad, I promise. I’ve found a lot of fear of hemodynamics comes from the basic terms never being clearly explained, and, luckily for you, I’m here to explain them simply.
Let’s start with defining each variable.
Systole: the phase of the cardiac cycle when the heart muscle contracts and pumps blood. When you hear the word systole, think about the heart contracting or squeezing. When the heart contracts and blood is pumped through the arteries, the pressure generated throughout the body is at its highest – this is what we call systolic blood pressure (SBP).
Diastole: the phase of the cardiac cycle when the heart relaxes and allows its chambers to fill with blood. The opposite of systole, diastole is the period where the heart relaxes. When the heart relaxes, the pressure in the body chills out as well – this is what we call diastolic blood pressure (DBP).
Blood pressure is represented by the systolic pressure over the diastolic pressure, with the textbook perfect blood pressure being 120/80 mm Hg.

Heart rate (HR)- a little straightforward, but hey, I’m not here to judge. Heart rate is represented as the number of times your heart undergoes systole, or contracts, or beats, or whatever you want to call it – per minute. That’s why we represent it in “bpm” – beats per minute. A normal pulse for healthy adults is anywhere between 60-100 bpm but can vary. Some athletes can naturally sit in the 50s and be completely fine (I definitely do not fit into this category).
Stroke Volume (SV)- remember how in the coronary anatomy overview we talked about how blood leaves the heart via the left ventricle and gets pushed out into the aorta? Well the amount, or volume of blood that the left ventricle pushes out per each beat is known as the stroke volume. So let’s say we’re in your left ventricle and your heart squeezes and 75 mLs of blood is pumped out into the aorta. The stroke volume in this example would be 75 mLs.
Ejection Fraction (EF)- Ejection fraction goes hand-in-hand with stroke volume. Picture yourself in the left ventricle (can you tell I’m a very visual person – I say stuff like this a lot 🤷♀️🤷♀️). At the end of diastole, or the relaxation period, the amount of blood in your left ventricle is known as left ventricular end-diastolic volume (also known as LVEDV). Ejection fraction is essentially the fraction of blood that is pumped out of your left ventricle during systole over the total amount of blood in your left ventricle prior to that contraction.
When your heart contracts, it’s not normal for the left ventricle to expels ALL of the blood that is within it – in fact, it’s basically unheard of. Instead, it usually ejects about 60% of blood out into the aorta.
To see it more visually, the formula for ejection fraction is:

So – let’s nail down the concept of ejection fraction with an example.
This is not realistic, but for the purposes of explanation let’s say your left ventricular end diastolic volume (LVEDV) is 1,000 mLs.
Let’s say 500 mLs of that blood is pumped OUT of the left ventricle during systole.
- What would the ejection fraction be?
- What would the stroke volume be?
If you said that the EF would be 50% and the stroke volume would be 500 mL, you would be correct.
Keep in mind the ejection fraction is exactly what it sounds like – a fraction – which means that everything is relative and proportional.
If you had a patient who had a left ventricle that only could hold 5 mL and they expelled 2.5 mL versus a patient whose left ventricle could hold 2,000 mL and they expelled 1,000 mL – despite these large differences in blood volume, both of these patients would be considered to have an EF of 50%. This concept will be important to understand as we talk about heart failure later.
Systemic Vascular Resistance (SVR): the amount of force exerted on circulating blood by the vessels of your body. Think of SVR as the amount of “clamping down” your vessels are doing.
Now that we have the basic terms down, let’s discuss hemodynamics.
Cardiac output (CO) is the amount of blood that leaves the heart per unit of time. Because of this, cardiac output is a good marker of our body’s total perfusion (aka the passage of blood through vessels in an organ or tissue). Think about our definitions above. This is why cardiac output is defined as:
CO = HR x SV
Both of these variables (HR and SV) are really important to define cardiac output. Afterall, if a patient had great stroke volume (aka the amount of blood they can pump out during each beat is a good amount) but they only had a heart rate of 43 beats per minute – they really wouldn’t be getting enough blood out of their heart to feed their organs, would they?
On the converse side, if a patient had a heart rate of 90 beats per minute but had a very small stroke volume, the amount of blood reaching the organs would also not be optimal.
However, cardiac output as a value can be a little tricky to interpret quickly. For example, if Dwayne the Rock Johnson and I were both in the Cardiac ICU at the same time, a cardiac output of 5 L/minute may be enough to sustain someone like me (sidenote: I’m not muscular or 260 lbs) but may not be enough to sustain someone like The Rock.

That is why the Cardiac Index (CI) was invented. The cardiac index is an assessment of the cardiac output that standardizes cardiac output based on a patient’s size.
The formula for cardiac index is:
Cardiac Index (CI) = (Cardiac Output) / (Body Surface Area)
Thanks to the Cardiac Index, if you told the rounding doc that my CI was 3 L/min/m2 and the Rock’s CI was also 3 L/m/m2, they could automatically assess that both of our cardiac outputs are adequate for our sizes.

Next let’s talk about the formula for blood pressure.
Blood pressure is the force of your blood pushing against the walls of your arteries. Note that this is different from SVR – SVR is the force that your vessels exert on your blood.
There are two main factors to consider when we are thinking about blood pressure – volume and squeeze. I like to think of blood pressure using the “water tank” analogy. In order for the water generate a force, you first need to fill the tank with water itself. Without water, there is no pressure.
Then, the pressure the water exerts against the walls of the tank will determined by how narrow or wide the tank is. The wider the tank, the less pressure the water would exert against the walls of the tank.
The more water, the higher the pressure. Similarly, the smaller the container (tank), the higher the pressure.
The water in this analogy is your cardiac output and the size of the tank is your systemic vascular resistance.
Therefore, the formula for blood pressure is:
BP = CO x SVR
Next, let’s talk about MAP.

No, not that type of MAP.
MAP stands for mean arterial pressure and is basically the average amount of pressure your arteries see during one cardiac cycle.
Wait a second – didn’t I just tell you that your arteries experience different amounts of pressure depending on if your heart is in systole or diastole? Pressure tends to be higher during systole and lower during diastole.
MAP takes all of this into account.
If you think about it, does your heart spend most of its time contracting (systole) or relaxing (diastole)?
If you guessed diastole, you’d be right. Afterall, your heart needs to give itself time to fill with blood while relaxing before pushing that blood out. In fact, on average, our heart spends 2/3rds of the time relaxing and only 1/3rd of the time contracting. Which is why the formula for MAP is:
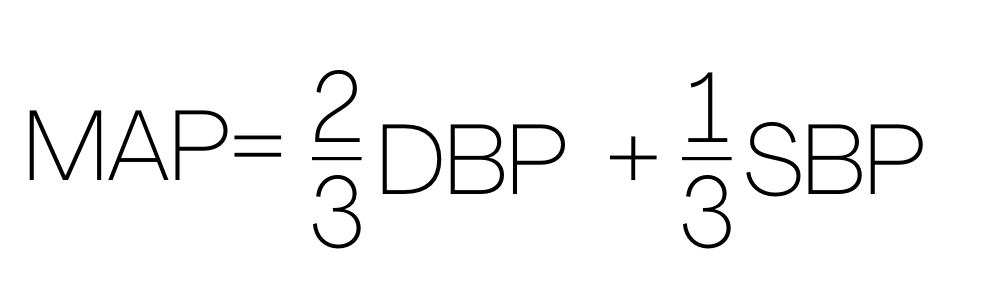
In the critical care setting, we like to go by MAPs often since it gives a more holistic view of perfusion. In fact, your diastolic blood pressure actually contributes to your MAP more than your systolic blood pressures. Some patients have weakened hearts that are unable to generate high forces of contractions, so their SBPs may not be high but their MAPs may still be fine since they are maintaining a good diastolic pressure. Generally, we target at least a MAP of >65 in the intensive care setting.
Stay tuned for a post describing the differences between preload and afterload!

3 thoughts on “Hemodynamics – The Basics”