I hope everyone had a very great and safe COVID-friendly holiday season. Happy 2022. Here’s to hoping for some brighter days in healthcare.
Today we’re going to talk about a very integral hormone system our body possesses that is at the heart (get it 😏😏) of understanding cardiology. And before we start talking treatment of heart failure, I want to talk about the RAAS.

Just like a lot of other things in school, I feel like the RAAS is something I begrudgingly memorized. But if you break it down to the basics, it becomes more digestible.
In order to understand the RAAS, you first have to understand why the heck our body even has this system.
The whole purpose of the RAAS is to regulate blood pressure. In order to do this, the RAAS works to alter 1.) blood volume and 2.) systemic vascular resistance.
This system starts all the way in the little beans we call kidneys.
Listen, I’m no kidney expert, and I know this is supposed to be a CARDS blog but the heart and kidneys are very closely intertwined.

If you’re anything like me, I didn’t like nephrology in school because I really didn’t appreciate it for what it was. However, the kidneys are extraordinarily important to regulate blood pressure.
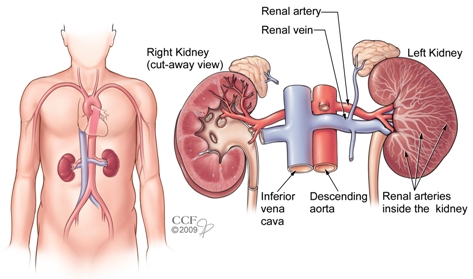
Let’s first get you oriented with how blood flows to the kidney. Oxygenated blood goes out of your LV and out to your aorta. Directly branching out of your abdominal section of your aorta are the renal arteries (one for your left side, one for your right side).
These large vessels then branch into smaller and smaller arteries until the blood reaches what we call the nephrons, or the functional units of the kidney. You can kinda think about a nephron like how we think about a cheeseburger. A cheeseburger is made up of different, smaller parts (the bun, patty, and cheese) – and without any of these ingredients, it wouldn’t be a functional cheeseburger – it would just be….a hamburger…grilled cheese…or some healthy keto-thing.

The nephron is how we decided to name a functional unit of the kidney but the nephron is made up of multiple different elements.
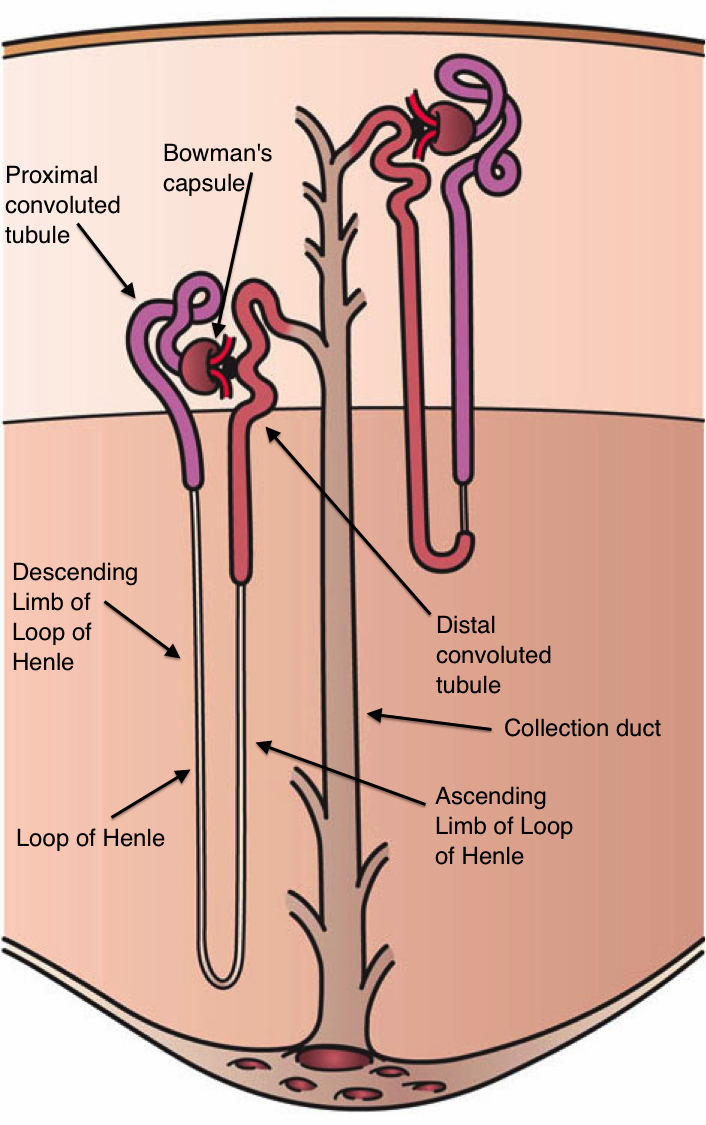
Each nephron consists of a renal corpuscle and a renal tubule.
The renal corpuscle is made of a knot of capillaries known as the glomerulus surrounded by a double-walled capsule known as Bowman’s capsule. The Bowman’s capsule is the area where the blood from the glomerulus is filtered to produce tubular fluid which will eventually become urine.

The name of the arteriole that enters the glomerulus is called the afferent arteriole and the name of the arteriole that leaves the glomerulus is called the efferent arteriole (e=exit).
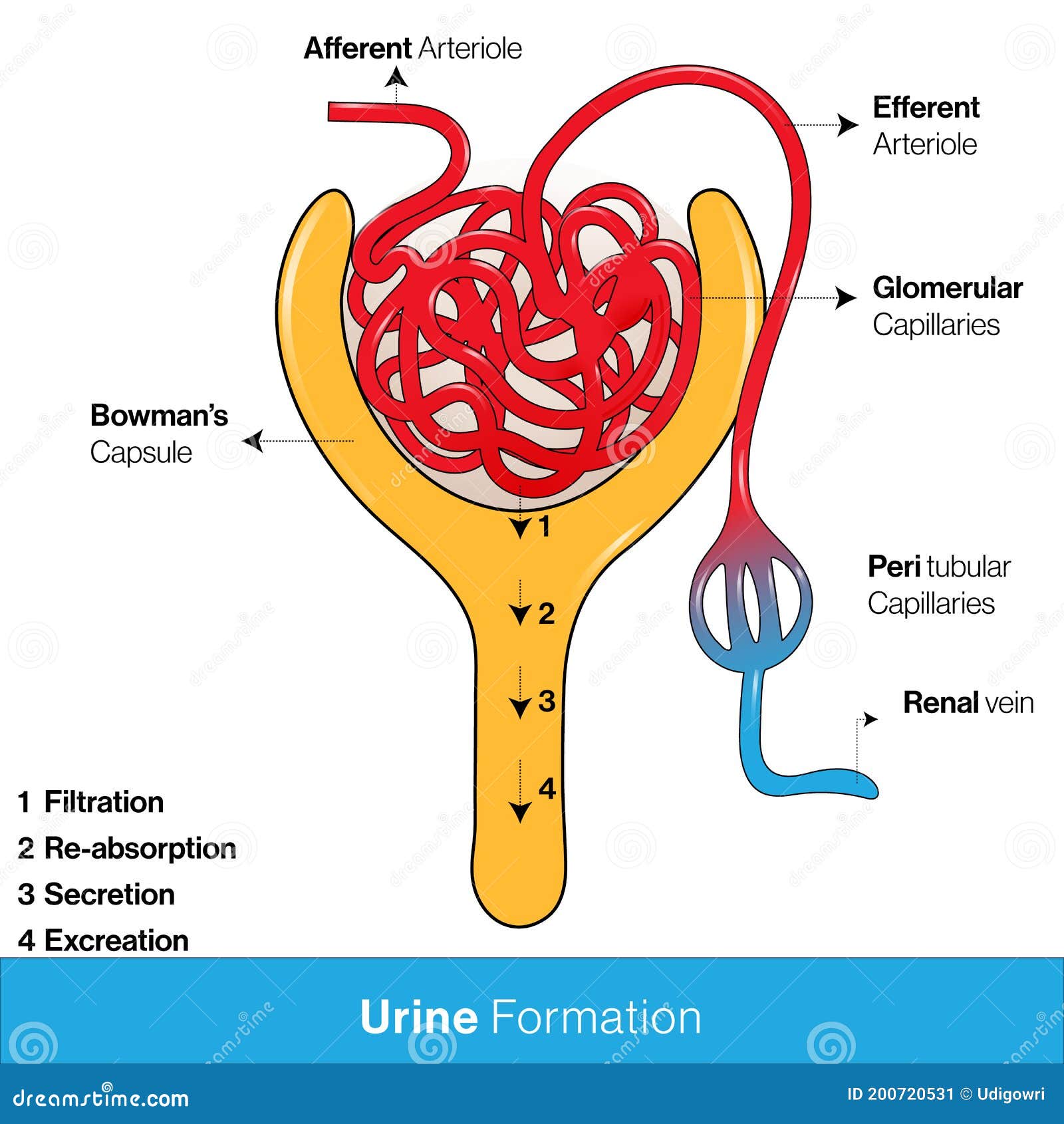
Meanwhile, the now-filtered blood will exit the glomerulus through the efferent arteriole. The efferent arteriole will eventually become the peritubular capillaries which will then turn into the renal vein. The blood from the renal vein will then collect and feed back into inferior vena cava (IVC).
So to reiterate – oxygenated blood goes from the LV -> aorta -> renal artery -> smaller and smaller arteries -> afferent arteriole -> glomerulus (blood gets filtered out here – some of it will come out into the tubules to become urine, and the rest will then go to the) -> efferent arteriole -> peritubular capillaries -> renal vein -> IVC -> 🫀.
Now that we got blood flow down, let’s talk about what happens to that tubular fluid that was filtered out from the blood in the Bowman’s capsule.
Remember those renal tubules I talked about before? The renal tubule is made up of distinct sections that will influence the body’s electrolytes and volume. For the purpose of today’s talk on RAAS, that’s all I need you to know.
Within the walls of your afferent arterioles, are a type of cell known as the juxtaglomerular cells. These cells are able to synthesize, store and secrete an enzyme we call renin.
When blood pressure is low or renal blood flow is reduced, your juxtaglomerular cells secrete renin in response to that drop in blood pressure detected by stretch receptors in the vascular walls. The juxtaglomerular cells can also be stimulated to release renin by macula densa cells. The macula densa cells are located in your tubules and will stimulate the juxtaglomerular cells when they detect decreased delivery of Na+ and Cl- ions in the tubular fluid.

The juxtaglomerular cells secrete renin directly into circulation. Once in plasma, renin serves as an enzyme and converts angiotensinogen to angiotensin I.
Angiotensinogen is a protein that is secreted by the liver.
Angiotensin I doesn’t really have much biological activity itself, and exists as a precursor to angiotensin II.
Once in the bloodstream, angiotensin I gets converted to angiotensin II by an enzyme called angiotensin-converting enzyme aka (ACE). ACE is found in the endothelial cells of capillaries and within the lungs.
Believe it or not, all this work is to make angiotensin II – which is the one of the major bioactive products of this system.
Angiotensin II has a few main biological roles.
- Angiotensin II binds to intraglomerular mesangial cells which are in the glomerular capillaries in the kidney. These cells help to regulate glomerular filtration rate (GFR), and when stimulated by angiotensin II, contract and reduce GFR. Why? Think about it, if your body senses low blood pressure, it’s going to want to reduce volume loss. By reducing GFR, you are reducing the amount of volume within blood lost to the urine.
- Angiotensin II causes the release of aldosterone from the adrenal cortex, which is the largest part of the adrenal gland. Aldosterone is a mineralocorticoid (a type of steroid hormone that regulates electrolyte balance and fluid balance). Aldosterone increases sodium and water retention by acting on the tubules in the kidneys. By increasing water retention, your body can increase its circulating blood volume/prevent loss of further water and help to increase blood pressure.
- Angiotensin II causes the release of a hormone known as anti-diuretic hormone (ADH also known as vasopressin) from the pituitary gland. ADH also acts to increase water reabsorption in the kidneys.
- Angiotensin II binds to angiotensin receptors located in the vessel walls. This binding will stimulate potent vasoconstriction which will then increase systemic vascular resistance (SVR). There are also angiotensin II receptors located in the afferent arterioles in the kidneys. When stimulated, these afferent arterioles will also contract.
Think back to the formula for blood pressure that we discussed in our hemodynamics talk. Remember how both blood volume and vessel squeeze influenced blood pressure?
BP = CO x SVR
Well, as we talked about above, the RAAS system is going to increase blood pressure by increasing CO. Remember that CO = HR x SV. By increasing the amount of circulating blood, SV will be increased which will in turn increase CO.
The RAAS system will also serve to increase SVR by binding to the angiotensin II receptors and inducing vasoconstriction.
So in reality, the RAAS system is doing exactly what I told you it would do – it serves to increase blood pressure by increasing both SVR (through the action of angiotensin II) and cardiac output (by increasing circulating blood volume through the work of aldosterone).
Drugs that influence the RAAS
Listen, once we figured out this biologic system, we quickly figured out we could use it to our advantage and alter it at different points to induce effects we want to see in our patients. We will talk about these meds in a future post.



Everything is very open with a really clear description of the challenges. It was really informative. Your website is very useful. Many thanks for sharing!
LikeLike