Hey all. Figured it would be a good time to talk about something that I used to hate – the cardiac action potential and ion movement through the ventricular myocytes. This will be key when we start talking about some of our antiarrhythmic agents (bum bum buuuuummmmmmmm)!
First thing’s first. Let’s start with the basics. In your heart, there are two main types of cells:
- Conduction cells ⚡
- Muscle cells (cardiomyocytes) 💪
Your heart is triggered by electricity (pretty cool I know).
The conduction cells are responsible for carrying the electrical signals throughout your heart to then trigger your cardiomyocytes to squeeze so your heart can do its thang.
So to repeat – conduction cells bring electrical impulses down the heart; those impulses trigger the cardiomyocytes to contract and all is well in the world.
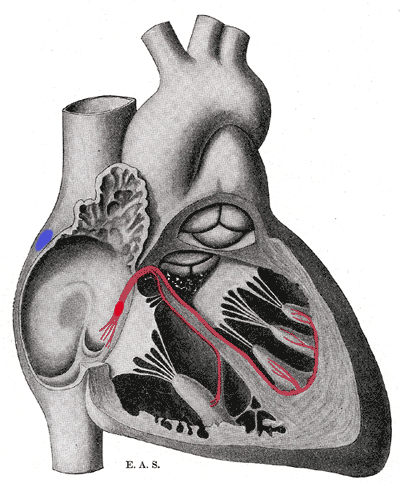
⚡The Conduction System⚡
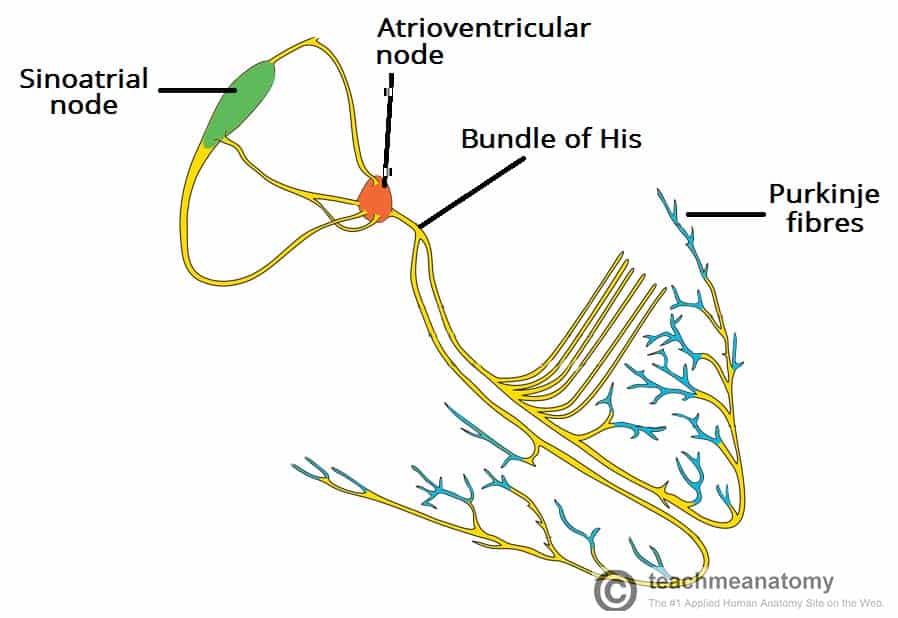
First let’s talk about the pathway that your body uses to normally send electricity throughout your heart.
It all starts at the sinoatrial node (SA node). The SA node is a special group of conduction cells located in the right atrium of the heart (fun fact – the SA node is 🍌 shaped). The SA node serves as your heart’s natural pacemaker of your heart, since in a healthy heart, it continuously sends off electrical impulses and sets the rhythm of the heart (AKA sinus rhythm).
The rate at which the SA node fires (aka the heart rate) is a result of the activity of two sets of nerves – the sympathetic nervous system and the parasympathetic nervous system.
The sympathetic nervous system (think fight or flight) stimulates and the SA node to speed up firing, and the parasympathetic nervous system (think rest and digest) stimulates the SA node to chill down and slow down conduction.
Any rhythm that starts at the sinus node is a considered a “sinus” rhythm.
The firing of the SA node causes the atria (upper heart chambers to contract).
That conduction signal then moves down the pathway (check out the diagram above) and moves down to the aptly named atrioventricular (AV) node. As the name suggests, the AV node is located in the septum in between the right atria and the right ventricle.
The AV node is prettttty cool in that it actually purposefully delays impulses (by ~0.09 seconds).
Why??
This delay is actually super important as it allows time and ensures the atria have ejected out their blood into the ventricles first before the contraction of the ventricles.
In other words, if we didn’t have this natural delay that the AV node causes, we might not get enough blood into our ventricles before the ventricles contract.
The AV node also serves as a protective step to protect your ventricles from beating way too fast in response to any type of atrial arrhythmias. She’s a keeper.
Take your Afib patients for example – in atrial fibrillation, the heart tissue is sending inappropriate electrical signals in the atria. These points of ectopy (aka these wrongly placed firing signals) are causing the atria in these patients to quiver. These afib patients are all out there in the community with their left atrias bajillion (kidding) ectopic points all firing and fibrillating though.

But the majority of these >4 million Afib patients are still doing their thing in the US and going about their normal business. Couldn’t be bothered.
Why? It’s all thanks to the AV node.
If those atrial impulses ended up going to the ventricles, you would end up with issues like Afib with RVR (atrial fibrillation with rapid ventricular response) which is more of a big deal causing symptoms and even hypotension in our patients – this is an example of where we might pull out the big gun and ⚡⚡shock⚡⚡ the patient back into normal sinus rhythm (NSR).
Hopefully that makes sense because it’s one thing for your atria to be quivering – atrias don’t have much of a contraction at baseline and a lot of the blood flow through the ventricles is passive….but if your ventricles are quivering or rapidly beating..that’s a different story. Your ventricles are so key in your body. They possess the force needed to squeeze blood through the lungs and to the body, and if they don’t squeeze – you don’t perfuse. This is why run of the mill Afib isn’t a huge deal, but you get a patient in pulseless Vtach or Vfib and that’s an indication to start CPR.
TLDR: It’s all fine and dandy (to an extent) when your atria alone are quivering. But if those signals get conducted to your ventricles – you are not going to get blood out to the body – and that patient is in trouble.
OK so recap – SA node fires, atria contract, meanwhile that impulse travels down the conduction cells to the AV node which waits a teeny bit of time before letting that impulse travel further down to ensure your atria are complete done contracting and filling blood into the ventricles.
Another amazing quality of the AV node is that it has decremental conduction – aka the faster it gets stimulated, the slower it conducts. This is (once again) what saves most people from having rapid heart beats/ventricular rates during periods of rapid atrial rhythms like atrial fibrillation or atrial flutter. The AV node is seriously the MVP.
The AV node‘s firing rate in and of itself (without any stimulation from the SA nodes) is about 40-60 times/min. Listen, our body is pretty incredible, and as such, has built in a lot of important “back up” systems to keep you alive in the case of something failing. It’s super redundant – and it might just end up saving your life.
This means that even if you have damage and lose all sense of conduction from the SA note, the AV node will still keep the body alive by pacing the ventricles (albeit slower – but enough to keep you alive in the meantime) and getting blood to leave the heart.
So besides serving as a signaling connection between your atria and ventricles, your AV node does two important things:
- Synchronizing atrial->ventricular contractions by creating a lil’ delay to ensure the atria are done doing their thing and spitting their blood into the ventricles
- Protecting the ventricles from rapid atrial arrythmias
(oh, and you know, keeping you alive if your SA node messes up). Casual.

Now moving on to the Bundle of His. I know what my fellow feminists are thinking – why not bundle of Hers? But, to be fair, the bundle of His is named after its discoverer Swiss-born Wilhelm His Jr.
The bundle of His is an important part of this whole conduction cycle as it transmits those electrical signals from the AV node to the ventricles of the heart.
The bundle of His breaks off into two different segments – the left bundle branch and the right bundle branch.
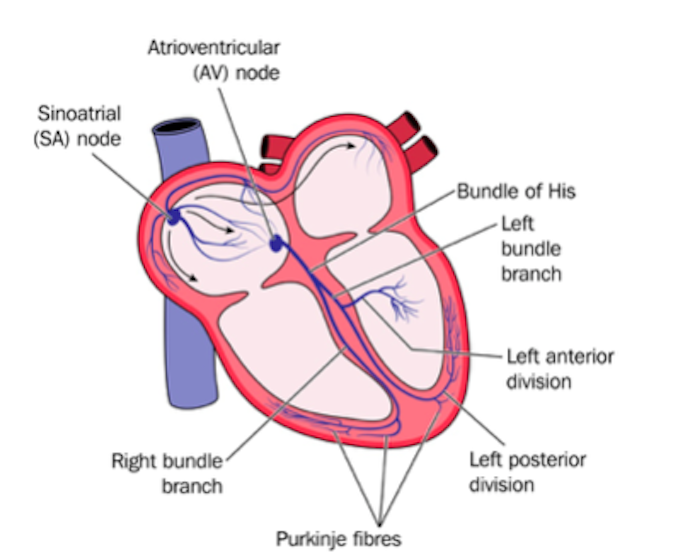
These left and right bundle branches run along the septum of the ventricles. Eventually these branches break off into teeny tiny thin filaments known as the Purkinje fibers. The ventricular conduction system is made up of both the bundle branches and the Purkinje fibers.
As the bundle branches and the Purkinje fibers receive the electrical impulse, the ventricles contract. As they contract, keep in mind (based on our coronary anatomy) that blood will be pumped from the RV to the pulmonary arteries and from the LV to the aorta.
OK let’s say shit has gone down and now your SA node isn’t working, your AV node is out, and even your bundle of His is down. The Purkinje fibers have the ability still take over with automaticity, but their natural rate is super lower, their minimum heart rate will be around 20-40 bpm.

OK – time for your first break. Get a glass of water, stretch it out, go for a walk. Come back to this page tomorrow if you need to. Here’s a pic of my chunky dog Ashe to break things up:

The Nitty Gritty
OK – Here’s are when things get a little more squirrelly and complicated because it’s fairly detailed so it’s best to have a fresh mind.
Remember when we talked about how there are two main cardiac cells – the cardiac myocytes and the conduction system cells/pacemaker cells?
Well, they actually have different mechanisms that cause them to fire or contract (in other words, go through an action potential). An action potential is defined as a change in the electrical potential associated with an impulse passing through a membrane of a cell. When the relative concentration of the cell goes from negative to positive, the cell depolarizes (aka the movement of the cell’s membrane potential goes to a more positive state) and when it returns to a more negative state, we call this repolarization.
Today I want to talk about the action potential of our cardiac myocytes, since this will directly translate when we start talking about antiarrhythmics.
Before we talk about the action potential of the cardiac muscle cells, I want to review what happens in the cardiac cycle. When the heart contracts, I want you to remember that first the atria (upper chambers) contract pushing the blood down through the tricuspid and mitral valves into the ventricles.

Next, the ventricles contract, pushing their blood up and out to the arteries (to the pulmonary arteries on the right side, and the aorta and out to the body on the side).
In other words, the heart contracts the atria…..waits…..and then contracts the ventricles.

But in order for the heart to contract, it needs a signal – something to tell it that it’s “go time” to do its thing. We’ll get to that soon.
When you look at pretty much any cell of the body at baseline – there is an an overall negative charge inside of it relative to the charge outside the cell.
All these cells have something called the Na+/K+ ATPase pump that takes 3 Na+ OUT of the cell and puts 2 K+ INTO the cell.
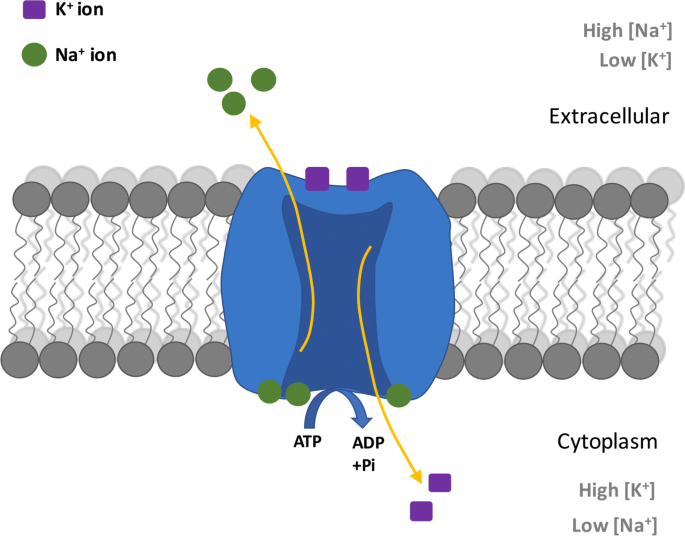
Because of this, your net charge of your cells relative to the outside is going to be negative (afterall you have more positive ions leaving the cell than coming into the cell).
This is why, at baseline, all cells are net negatively charged within the cell and the outside of the cell is net positively charged.
Keep in mind that the movement of ions across cell membranes within the body all boils down to the law of diffusion, the idea that ions want to go from a level of higher concentration to lower concentration to create, if possible, an equilibrium.
And also keep in mind because of all these bajillion Na+/K+ ATPase pumps keeping cell membranes net negative – they also create a high concentration of Na outside of the cell and a low concentration of K outside of the cell.
When I was in school, I always forgot which ion moved what way. Now as a baby practitioner, I can offer you my trick of what’s a practical, real-life thing that can help you remember.
My trick is thinking back to our normal basic metabolic panel (BMP).
What’s a normal Na value in blood? 135-145 mEq/L right? That’s pretty darn high.
And what about K? Only about 3.5-5 mEq/L right?
And what happens when you get a sample of hemolyzed blood that was damaged and caused cells to lyse open? You get these wonkily high K+ levels right? That’s because the K+ is so much higher intracellulary.
Since the level of K is low in the blood, this must mean that the Na+/K+ ATPase pumps potassium INTO the cell, causing high intracellular concentrations of K (and low extracellular concentrations that we see on BMP). On the flip side, Na values in the BMP blood are fairly high, meaning that sodium levels within the cell are low. And this is all thanks to that Na/K ATPase pump.
However, remember that the cell membrane is made up of fats, and ions can’t freely pass/diffuse through fats. So if ions come into contact with the cell membrane surface, they’ll just bounce right off.

The only way for these ions to move in between the intracellular and extracellular space is through channels, or basically these special doorways that they can use to access the inside (or move the outside of the cell).
Besides the Na/ATPase pumps, on the surface of the myocardium muscle cells, we have special channels that show allow only certain ions to pass when they open- we have channels specifically for Na+, and channels specific for K+.
Cardiac muscle cells ultimately want to contract, right? Well, when they aren’t contracting (aka they are at rest), you’ll find that the sodium channels on the surface of the cell are closed. This means that the sodium that’s outside of the cell (at high concentrations) is trapped there right? It can’t get into the cell because the sodium specific channels are closed. Because the channels are closed, the Na/K ATPases throughout the cell are keeping that cell at a net negative resting state.
This concept is so important to understand – that a cardiomyocyte has to, at rest, be negative – because if it wasn’t it would not be able to contract.
If we were to take out a chunk of heart muscle and put it under a microscope, you would find that all these muscle cells sit closely together, side by side, and are connected by a series of gap junction channels. The purpose of gap junctions are to provide direct contact between cardiac cells so that these waves of depolarization spread rapidly throughout the whole heart and pass from cell to cell quickly.
When these myocytes get stimulated by the pacemaker cells – the cell gets triggered that it’s “go-time” and the Na channels will open up.

These Na channels will begin to leak positive sodium ions into the myocyte cell and when that first myocyte reaches -70 mV, all the rest of the Na channels will take that as their cue to pop open up.
Now, with ALL these sodium channels open, sodium will rushhhhhhhh into the cell; and as those positive ions rush in the electric potential of the will SHOOT up and become positive. This is called depolarization.

So in other words, the Na+ channels will open. The high concentration of Na extracellularly (thanks to the Na/K ATPase pump) will want to diffuse into an area of lower concentration (aka the inside of the cell).
However, keep in mind that these myocytes are connected by gap junctions. As soon as one muscle cell depolarizes, because each muscle cell is physically connected to the next, some of the sodium from the first cell will trickle into the cell next to it.
So that next cell becomes more positive, hits -70mV, and then that cell will flip off all of its Na channel lids and Na will trickle in and so on and so forth as it moves through all the cells.
This domino effect basically means when one muscle cell depolarizes, it will spread a wave of depolarization throughout the rest of the muscle cells through Na trickling into the next cell via gap junctions.

Now once depolarization has occurred – all the Na+ channels are open and Na has come in – the cell’s potential will reach +10-+30 mV.
This +10 to +30 mV charge triggers all those Na channels to shut and close their lids.
At this point, remember that even with the Na+ lids now closed, the charge of the cell is very positive (literally, like +30mV) and so everything needs to reset. Somehow we have to figure out a way for our cell to get back negative/back to baseline.
This is where our K+ channels we talked about before start to open up/work.
Because the concentration of K is so high in the cell, these positive K+ ions will leave the cell and leak out, making it more negative inside the cell.
And so the graph of charge will start to dip a bit.

However something else happens now! There is one more channel you need to be aware of – the calcium channel. As the K+ leaks out, the Ca+2 channels open up and Ca+2 will start to move in.
I know what you’re thinking – you told me about the sodium channels, you told me about the potassium channels, but what is with these calcium channels coming in last second now? I’m annoyed.
OK well keep in mind that these are MUSCLE cells, and deep in the dirty cobwebs of your sleep deprived brain, you might remember that muscle cells have actin and myosin filaments that need to come together and literally need to “walk” across each other to contract that muscle.

The 🔑 to have this work is calcium.
However, because we still have the K+ channels open (making K+ leave the cell) and now Ca+2 is entering the cell, we overall have this plateau period in the cells of the myocytes.
The calcium channels like to do their thing and then get out of there – so they close fairly quickly and shut off.
The K channels still remain open and K continues to leave the cell, making the cell more negative and back to resting potential.
K+ channels will then close and the Na/K ATPase pump will keep going to keep that cell in resting potential, until the process starts all over again when it receives an impulse.
OK. Phew.
[Insert break # 2 here] – seriously. Clear your mind of all the things, watch Bridgerton, go bother your roommate. Below is a photo of my parent’s not chunky dog Zoey –

Now that we talked about this, let’s look at what this looks like visually.
I give you – the cardiac action potential of the myocyte.

There she is ^^^. Since the cardiac action potential is made up of different parts, we gave special names to each phase. We have phase 0, phase 1, phase 2, phase 3, and phase 4.
In this diagram, the green represents phase 0, yellow phase 1, blue phase 2, orangey/brown phase 3, and red phase 4. Let’s get into the deets.

Phase 0: Phase 0 is where rapid depolarization and increase in positivity happens (I mean look at that diagram).To get this thing positive, Na+ channels are going to open on the myocyte surface, creating an influx of Na+ into the cell (because once again we have high levels of Na+ outside the cell- think back to our lab values 135-145 mEq/L). This will lead to a quick uptick in a more positive membrane potential and actually get us to our highest peak of depolarization.
Phase 1: This is where we start to slow our roll and start repolarizing.

In Phase 1, we want to start getting the cell back to a more negative state so hopefully it should make sense that our Na+ channels are going to become inactivated, preventing more positive Na+ from going into the cell. At the same time, our K+ channels will begin to open, which will trigger the high amount of intracellular K to start moving OUT of the cell, making the cell less positive.

Next we have Phase 2. This is our plateau phase.
Keep in mind that at the beginning of phase 2, our Na+ channels are mostly closed (so preventing more positive Na+ ions from flowing into the cell) and the K+ channels will open (making more positive K+ ions leave the cell). If this trend continued, we would continually decrease our membrane potential to become more and more negative.
In phase 2, the plateau phase, Ca+2 channels will open and allow Ca+2 to rush into the cell. These positive Ca+2 entering the cell are going to balance the positive K+ ions leaving the cell – hence our plateau.

Phase 3: Also known as our rapid repolarization phase. In this phase we have massive K+ efflux (aka leaving the cell) due to the opening of slow delayed-rectifier K+ channels and the closing of the Ca+2 channels.
Phase 4: “Resting potential”

During Phase 4, we see high K+ permeability (going out of the cell) through the open K+ channels before those K channels shut. Now resting potential will be maintained by the Na/K ATPase pump until another impulse comes.
[Insert final break here!] You’re almost there! My husband and I have been working on redoing our guest bathroom. We decided on the below wallpaper last night (are we surprised):

The EKG
Let’s finish it up. One thing I didn’t realize for a long time is how the EKG corresponds to the cardiac action potential. I thought about them as two distinct things.
I’m about to combine those worlds.
When you hear the word depolarization, I want you to think about systole or squeeze. When you hear the word repolarization, I want you to think about diastole, or the period of relaxation.
We know that Phase 0 represents depolarization in the cardiac action potential, and we know that phase 3 represents repolarization.
This also translates to the EKG.
The QRS complex – the period of the EKG when the ventricles squeeze, is a physical representation of phase 0 of the cardiac action potential.
The QT interval – the period of the EKG where the ventricles relax, is a physical representation of phase 3 of the cardiac action potential.
This connection of ideas will hopefully make understanding antiarrhythmic agents so much easier.
So that was a lot. I hope you stuck with it. This is a dense talk, but hopefully you could follow along in the movement of ions and what is happening. Time and repetition will help you remember these things and help them stick. But the understanding of the actual process will help you a lot when we start talking about antiarrhythmic agents and their effects on things called the conduction velocity, the refractory period, and automaticity.

One thought on “The Cardiac Conduction Cycle and the Cardiac Action Potential ⚡⚡”