Today it’s time to talk about the most commonly encountered arrhythmia you’ll see in clinical practice – atrial fibrillation. There’s actually quite a lot to unpack here which is why I decided to break down Afib into three posts: an overview (hi, you’re looking at it rn), then treatments of the afib itself, and lastly anticoagulation.

Let’s.
Get.
Into.
It.
What is Atrial Fibrillation?
Atrial fibrillation, usually abbreviated a.fib., is a type of arrhythmia (irregular heartbeat) where the atria (upper chamber of the heart) fibrillate.
I like to think about fibrillation as a quivering. So, instead of having a nice lil’ coordinated contraction of that atria, you’ll instead end up with a trembling similar to Patrick’s lower lip – which leads to no coordinated contraction. It just kinda sits there and trembles.
If you think back to the EKG…..remember that there are the P, QRS, and T complexes. The P wave represents atrial contraction (depolarization), the QRS represents ventricular contraction (and also atrial relaxation), and the T wave represents ventricular relaxation.

Now, think back to what I just told you is happening in atrial fibrillation.
If you had a patient in atrial fibrillation….what part of the EKG do you think might be affected?

If you guessed the P wave….then you’d be right! If you guessed anything else, go and think about what you’ve done.
Because we don’t see that nice, coordinated motion of the atria contracting, the P wave will be absent on the EKG when a patient is in Afib. The other hallmark of the EKG in Afib is that you have an “irregularly irregular rhythm”.

In order for an EKG to be considered “regular”, the distance between the R to R intervals (peaks) have to remain consistent.
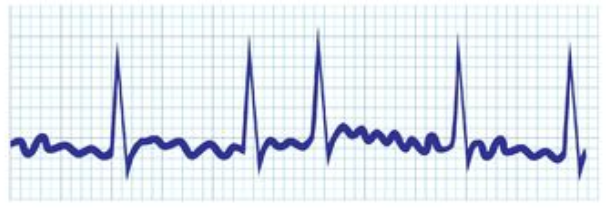
However, as you see in the example above, the R to R intervals are not just at different spacing, but they do not repeat in any pattern – hence the irregularly irregular rhythm.
What causes atrial fibrillation?
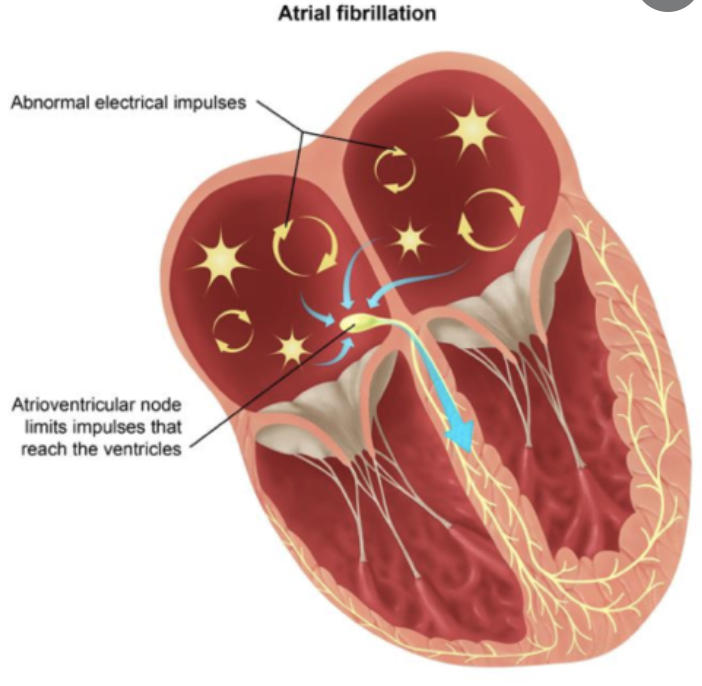
The foundational reason for afib is the presence of ectopic (aka in places where they shouldn’t be) conduction in the atria. In other words, instead of getting stimulation from the SA node alone, the atria are firing off at a bunch of random points within the atria.
Think of your atria basically having a 2000s rave. There’s just a lot going on, there’s a bunch of random lights – it’s not great.
But one thing I didn’t quite grasp in school is that there is about a bajillion causes of afib. Pretty much anything that mucks with or irritates that cardiac tissue can lead to afib. There’s also a difference between patients being in transient afib (aka short-lived, due to a distinct cause) versus having chronic atrial fibrillation.
For example, anything that goes in that area and touches/pisses off that tissue – whether it is a catheter or an invasive open heart surgery – can cause inflammation that can induce afib post-op. Patients with infection can also present in afib. If a patient is super volume overloaded, and they have atrial stretch, that stretching of that tissue can also cause those points of ectopy to start firing off. If this is the only cause, then often the patient might just be in short-term afib which will correct as that volume goes down or as that inflammation decreases. This is why in the hospital you might see a bunch of patients without a history of afib present to the ED in afib for the first time.

The major reason patients end up with chronic afib is due to any structural changes of the heart. Patients with a history of heart failure or valvular disease, for example may undergo structural changes to their hearts over time – the atria might start to balloon out and get thin, for example. This will cause these points of ectopy to form that likely won’t go away anytime soon (if ever), because the underlying cause – that change in the structure of the heart – is permanent.

As we get older, just like with anything else, our hearts also start to undergo structural changes over time. This is why the incidence of afib increases so much with age, with ~70% of patient in Afib between 65-85 years old. I mean I think that graph below speaks for itself.

Valvular Atrial Fibrillation versus Non-valvular Atrial Fibrillation
This topic is an active debate in the world of cardiology, and I’ve seen and heard a variety of definitions for what constitutes someone having valvular versus nonvalvular afib. The American AHA guidelines even says “the distinction between nonvalvular and valvular AF has long confused clinicians” 😂😂😂. That’s when you know it’s bad.
Valvular atrial fibrillation is defined as the presence of atrial fibrillation in a patient that has a mechanical heart valve and/or moderate-severe mitral stenosis.
If your patient has a history of afib and does NOT have a mechanical heart valve in any position and does NOT have moderate or severe mitral stenosis (aka a narrowing of the mitral valve), then they have nonvalvular atrial fibrillation.
(I’ll be explaining mitral valve stenosis briefly when we talk about anticoagulation and why these patients tend to get afib.)
This distinction among patients will become important as we talk about their treatments later on.
Types of Afib
Afib is further divided into categories based on timing.
Paroxysmal: refers to patients that have Afib that terminates either by itself (spontaneously) or with intervention within 7 days of onset. If you look up the actual definition of “paroxysmal”, you’ll find that it means a sudden attack or spasm.
Persistent: Continuous Afib for >7 days
Longstanding: Continuous AF for >12 mo
Permanent: this is basically when both a patient and their provider say that – we’re tired of trying to restore normal sinus rhythm (NSR)- we may have tried antiarrhythmics, or cardioversions, or ablation, but we’re just done. This is when the provider and patient accept that they probably won’t convert to a NSR anymore, and they agree to no longer pursue that option of treatment. Afterall, the longer a patient is in Afib, the less likely they are to be able to convert back.
Why do we have to treat Afib?
So, afib is very common, relatively speaking. There are literally millions of americans out there walking around in Afib.
So, what’s the big deal? Why do we have to do anything about it?
There’s quite a few reasons.
- We want to avoid atrial fibrillation with rapid ventricular rate (aka Afib w/ RVR)
Even though so many patients have their atria quivering out there, the reason these patients are stable is all thanks to their handy-dandy AV node. I like to think about the AV node as a lil gatekeeper of the ventricles. She works hard and works to prevent a lot of these random ectopic signals from reaching the ventricles. Afterall, the atria can be quivering at a rate of 300-600 times per minute. 😱😱😱 If those signals all reached your ventricles…you’d literally be dead (that’s basically what’s happening in Vfib…aka a cardiac arrest). Your ventricles would be moving so fast that they wouldn’t have good contraction and not be able to push blood out to the body. No blood = no oxygen = no life.
Now, under normal circumstances the AV node 🙅blocks🙅 those signals so they stay contained in the atria. In afib with RVR, some of those signals start passing through the AV node, and cause rapid contraction of your ventricles – luckily not at a rate of 300-600, but often reaching 180 bpm+. This can lead to hemodynamic instability as your ventricles start beating faster and faster, leading to less and less time to fill and may need urgent treatment.
2. We want to eliminate symptoms.
Some patients with afib may have no symptoms. But there are also a ton of patients out there that can get fatigue, palpitations, dizziness, fainting, etc. Not cool – I don’t know who wants those symptoms but definitely not me. Treatment can help eliminate or greatly reduce these symptoms of patients.
3. We want to prevent long term structural changes.

Ah yes, the age old question – what came first, the chicken or the egg?
We know that patients with heart failure can undergo structural changes that will then cause afib…but afib can also cause structural damage. It all boils down to the fact that your heart is a muscle – just like any other muscle in the body.
Now, I don’t go the the gym – but if I did – and I started to lift weights every day – what would happen to my biceps? They would probably grow right?
Your heart is the same. With chronic afib, your ventricles can often beat faster than normal and over time, the ventricles having to work harder will cause hypertrophy or growth of that heart muscle tissue. These structural changes can lead to heart failure or worsen pre-existing heart failure. No bueno.
4. We want to decrease the risk of strokes in our patients.
The slower blood moves, the more stasis it undergoes, the more likely you are to form a clot. In afib, we aren’t having our nice little contractions of our atria, helping to move that blood through our valves and into our ventricles.
Instead, that atria is just kinda sitting there, quivering. That blood that would normally be moving nicely is now kinda pooling around.
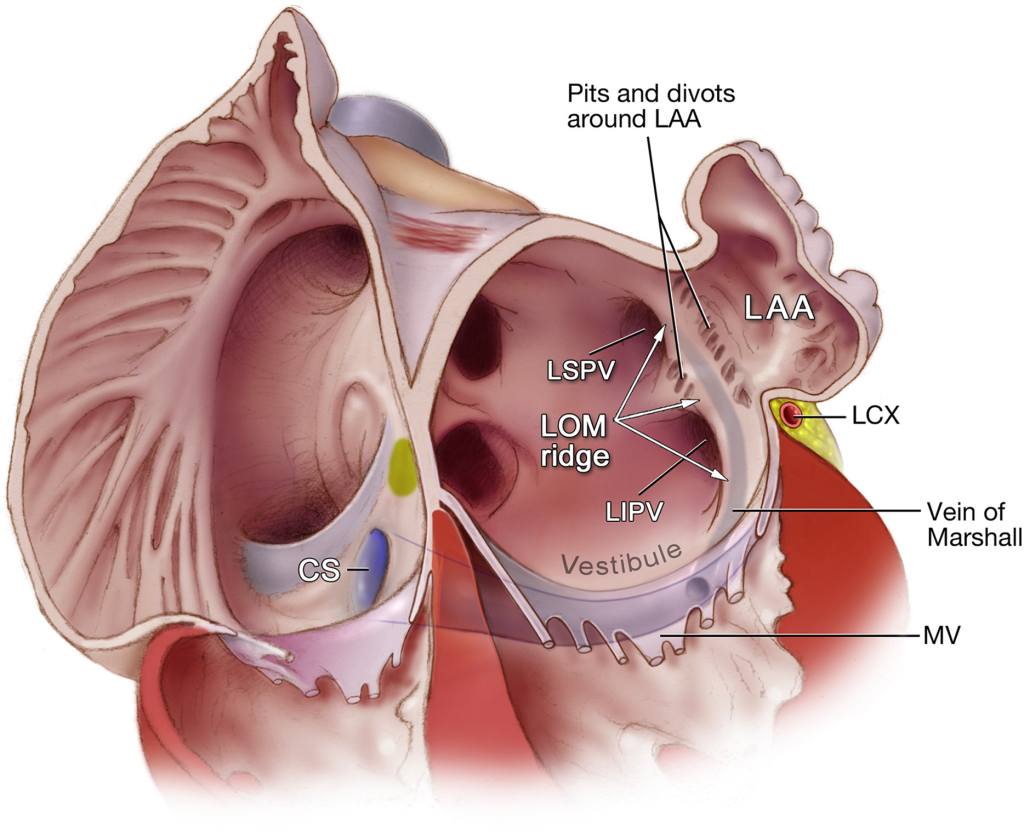
To make things even worse, we all have something called a left atrial appendage.
Now, we are all used to seeing the instagram-filtered pretty version of our heart:

But just like in life, keep in mind there is an instagram versus reality version of everything. The reality is that your atria has a big ol’ appendage sticking out of it. This is called the left atrial appendage, or LAA. Check her out below:
Fun fact: there are a lot of different names to characterize the shape of your atrial appendage. Some people have chicken wings, same have cacti, some have windsocks – there a lot. Check out some below:

I low key am so curious to know which one I have. This is what I lay awake at night and ponder.
Btw – totally just googled the below AND AM NOT ASHAMED TO ADMIT IT.

Anyway, the LAA becomes a really bad place to chill in when you have atrial fibrillation. In fact, it’s estimated that ~90% of all strokes from Afib originate in the LAA. Woof.
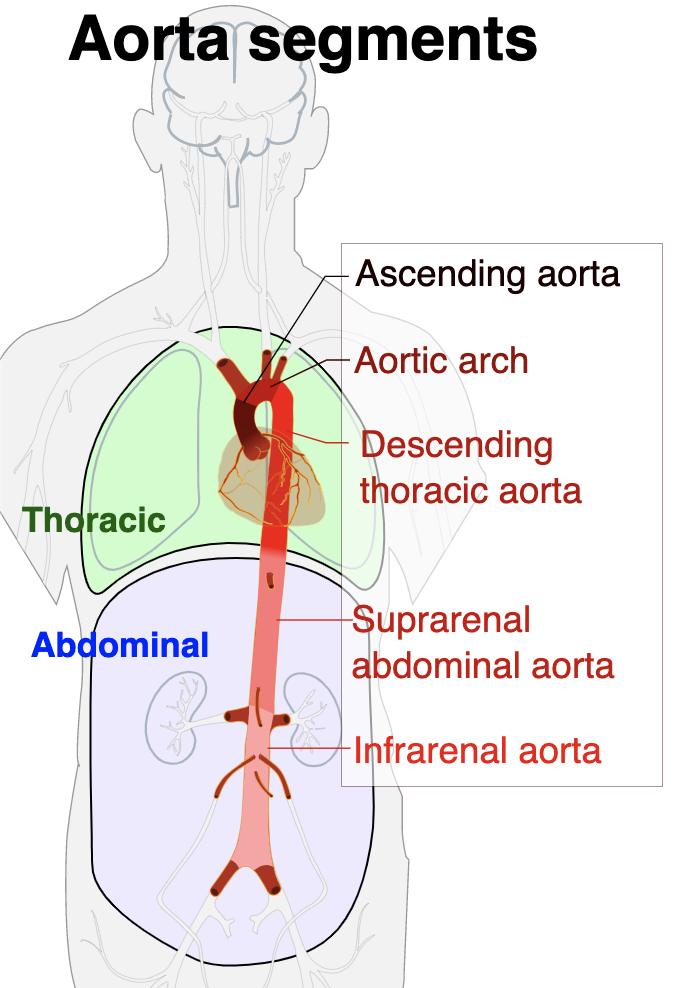
Now, if you recall the basic anatomy post, you’ll remember that if a clot forms in the left atrium, it’s going to travel through that mitral valve, through that left ventricle, out the aorta, where one of the first large branching of vessels goes up into the brain. This is why so many patients with atrial fibrillation get strokes. That clot can also opt to go further down into the aorta and get lodged in an artery throughout the body.
Just to solidify our knowledge of basic anatomy, it should hopefully make sense that that clot that forms in left atria would not cause a pulmonary embolism (PE) or deep vein thrombosis (DVT), however. That clot is going to go through the aorta, go into an artery and get stuck somewhere before the capillary beds. Afterall, the capillary beds are teeny tiny, so it’s literally impossible for that clot to somehow travel through the capillary beds and end up on the venous side of things (aka in the veins).
That marks the end of our basic overview! Next posts will be focusing on treatment – we’ll touch base on both pharmacological and nonpharmacological methods of treating both afib and preventing stroke in our patients.


4 thoughts on “Atrial Fibrillation: Overview”