Today we’re gonna begin to tackle a core cardiology topic: venous thromboembolism 🎉🎉. For the purposes of today’s intro, we’re going to focus on defining VTE, understand the anatomy, and nail down some core pathophys concepts before we get into more specifics in our future posts.
But before we dive into everything – you know me – we’re going to break down exactly what these words mean.

What is venous thromboembolism?
Let’s start with the basics: defining venous thromboembolism.
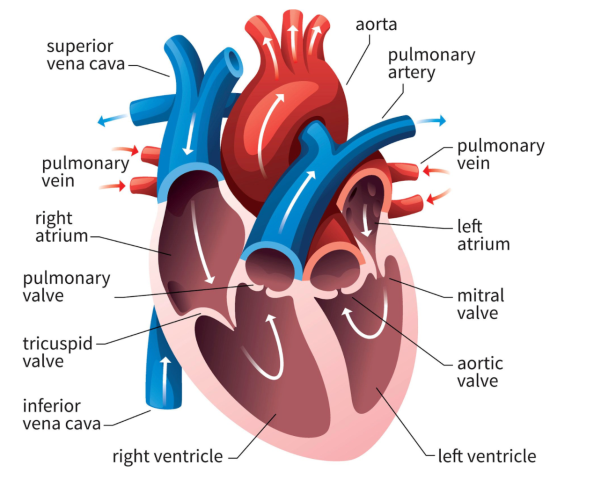
Venous, as the name suggests, pertains to the veins. For everyone who remembers our talk on basic anatomy/hemodynamics, veins are defined as vessels that carry blood back towards the heart. Most veins contain deoxygenated blood – but not all – the pulmonary vein is the exception to the rule – she carries oxygenated blood from the lungs back to the left side of the heart.
Thromboembolism is a combo of the words thrombus and embolism.
A thrombus is a fancy name for a blood clot.
A embolus is what happens when that blood clot (or a piece of that blood clot) breaks off and gets carried in the bloodstream and lodges itself in another area.

What falls under the category of a VTE?
Thromboembolism is a blanket term consisting of two main subtypes: you got your deep vein thrombosis and you got your pulmonary embolism.
A deep vein thrombosis, more commonly referred to as a DVT is when a blood clot (aka thrombus) forms in one or more of the deep veins of the body (usually in the legs). Key idea here is veins – not arteries.
A pulmonary embolism, commonly referred to as a PE, is when that blood clot gets stuck in an artery of the lung and blocks blood flow to a part of the lung. The majority of pulmonary embolisms start off as DVTs in the leg; those clots then break off and travel to the heart where they lodge in the lungs.
Why are DVTs and PEs considered VTEs but a stroke is not?
All of this goes back to basic anatomy, but I think it’s important to re-visit and re-remember so you can understand these concepts instead of memorize them.
Let’s revisit how blood flows in the body, starting with a vein in the legs. Let’s just pick a big one – the femoral vein.
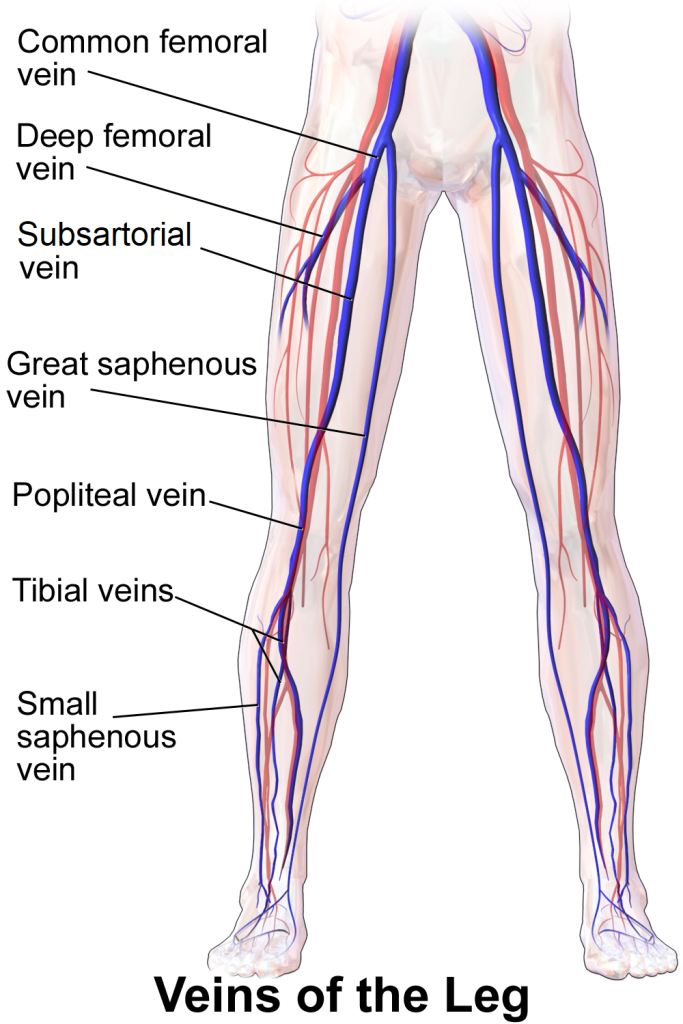
Alright let’s say a clot forms in your femoral vein (sorry, tough luck). Check out the diagram of the femoral vein to get an idea of where this clot is forming.
If that clot breaks off, where is it headed next? Well, first off, we know that clot is headed back towards the heart (since it is a vein, by definition of the word).

That clot is going to travel through the femoral arteries, through the iliac veins, and enter the big kahuna of deoxygenated blood flow – the inferior vena cava.
I like to think of the inferior vena cava as the superhighway vein of the lower part of your body – the smaller veins of your lower body will all deposit their blood into the inferior vena cava, the vena cava will collect all this blood, and then superhighway it back up to the heart.
The inferior vena cava then connects directly to the right side of the heart, and, you guessed it, it’s still carrying that pesky little embolus along for the ride.
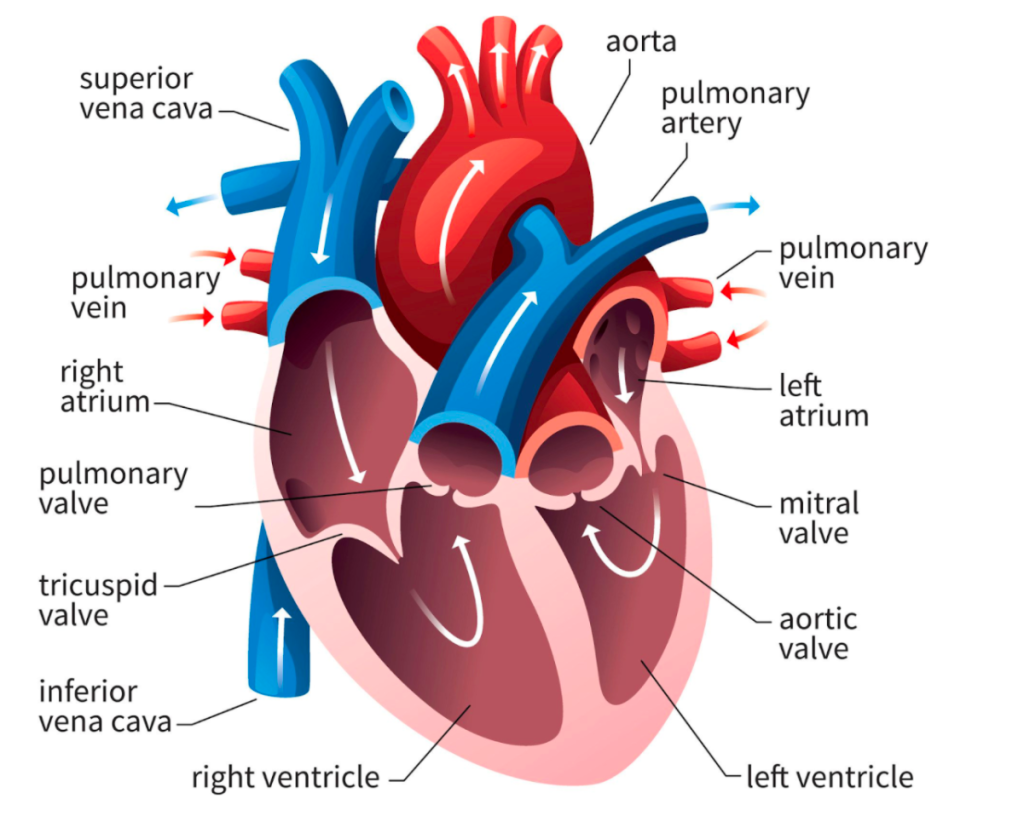
Once in the right atria, that clot is going to head through the tricuspid valve, through the right ventricle, and then go through the pulmonary artery into the lungs.
Now, remember that the pulmonary artery is going to break down into smaller and smaller vessels, eventually becoming teeny, tiny capillaries that wrap around each alveoli, and get oxygen.

In other words, in most patients, there’s absolutely no way a DVT is going to cause a stroke, since that DVT is going to embolize and get stuck either in the lungs or somewhere on the route before. If you remember, a stroke is an arterial-based clot, and usually comes from the left side of the heart, out the aorta, and up into the arteries that feed our brain.
Ok now time for a tangent 😈😈😈😈😈😈😈
Now, a little bit of extraneous information, but there is a way that DVT can cause strokes, and it all depends on your patient’s anatomy/structure of their heart.
Can you think of how the heck this would happen?
Well, I told you there’s no way that clot could pass through the lungs and get to the other side – to the left side of the heart – that sucker is going to get stuck in the lungs in those teeny tiny capillaries.
So how does this happen?
How does that clot go from the right side of their heart into the left side of their heart? The answer is simpler than you might think.
This can happen when there’s a literal hole in between the right and left side of the heart.
You heard me. A hole.

We call this hole a patent foramen ovale, or PFO.
Let’s back track a bit.
When we’re all lil guys in the womb, we need this hole (the foramen ovale) to bring blood from our right atria to our left atria – thus bypassing the lungs – since we’re aren’t USING our lungs in the womb – we get all of our oxygenation from our mother’s blood.
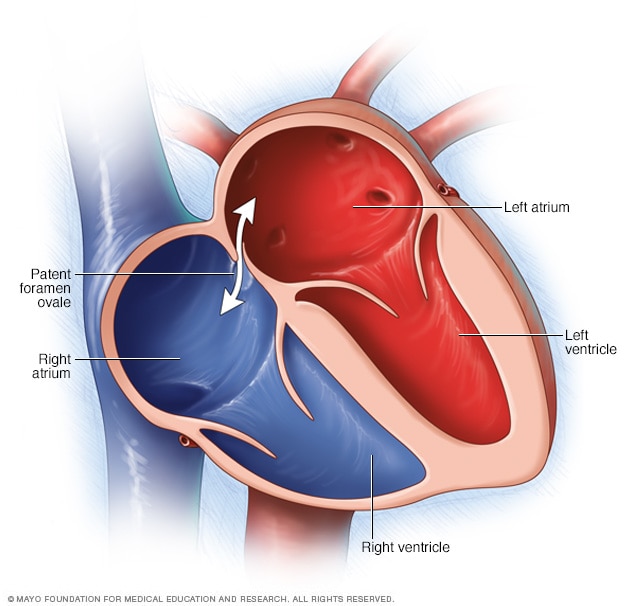
At birth, the foramen ovale is supposed to close up – but in about 25% of patients, it doesn’t completely close. In most patients, this isn’t an issue and nothing ever happens – in fact, YOU might have a patent foramen ovale right now reading this and you would never know.
However, if patients with a PFO have a DVT, they can end up getting what we call paradoxical embolism – where that clot travels from the venous side to the arterial side (because it pops right from the right side of the heart directly to the left) – and end up getting either a stroke, or an arterial clot somewhere.
We might test for a PFO if you are otherwise a healthy person without any other risk factors for stroke (e.g. no afib, for example) and present with a new acute ischemic stroke.
Can you think of how we might test for the presence of a PFO?
It’s too hard/small to necessarily visualize the hole itself on an ECHO (an ultrasound of the heart) but if we add a little ✨spice✨ we can.
Let’s add some bubbles to the mix.

Bubbles? Yep, you heard me. This test is called a bubble study, aka a saline contrast study.
Unlike Grey’s Anatomy or whatever other show you might have watched, a little air injected into our veins is really not a big deal – it doesn’t actually kill your patient or cause immediate arrest like popular culture might have you believe.
In a bubble study, your physician will take a sterile sodium chloride solution and *shake shake shake shake shake* until little teeny bubbles form and it’s all frothed up. They’ll then inject this into a vein.
Now following our anatomy, that solution is going to end up either in the SVC or IVC and enter the right side of the heart.
While this is happening, the doc will do an ECHO at the same time. The ECHO will enable them to physically see the air bubbles.

If the doc sees the air bubbles enter the RA, then the RV, and then…disappear? We’re good. Those air bubbles all went through the pulmonary artery (PA) and were expelled through the alveoli.
However, if the air bubbles all of a sudden end up on the left side of the heart? You’ve likely got a PFO, my friend.
I’ve always thought this test was so cool in its simplicity. A lot of medicine isn’t as “complex” as we might think it is – by using simple concepts, we can get some pretty powerful info out of it.
OK side tangent over.
Why are PEs dangerous? How can they kill you?
The last thing I want to introduce today is the concept of why a pulmonary embolism can kill your patient – and can do so pretty instantly. For those of you who are familiar with the advanced cardiac life support (ACLS) algorithm, you might remember that pulmonary embolism is one of the causes of asystole or pulseless electrical activity (PEA) in cardiac arrest.
Why does this happen? Do you just get deprived of oxygen because there’s a clot in your lungs and some of that blood can’t get enough O2? Did the clot block all of your blood flow?
So, it is possible for the clot to just be SO large that it traps itself and blocks off your pulmonary artery, preventing forward flow. This is rarer, but as you might believe, causes pretty instant death.
The main reason we see PEs being so dangerous are actually due to the effect that the clot has on the right side of the heart.
What effect do you think that clot in your lungs has on your right heart?
Well, let’s go back to the idea of simple physics and what happens when a fluid tries to go through a smaller space. What’s going to happen to the pressure before that blood clot?
As less blood is able to travel easily through the lungs, more blood is going to get “backed up” and the pressure of the structures PRIOR to the clot is going to INCREASE as a result.
If you think back to your simple anatomy, the RV sits prior to your pulmonary vasculature. As that clot blocks blood flow, the pressure in your RV is going to get higher…and higher…and higher.
Depending on how high the pressure is, your RV might still be able to push through that pressure. But if it gets increasingly higher, we will start seeing physical changes in your heart from this increase of pressure.
As that pressure increases, your RV is actually going to start growing and cause what we call “septal bowing”. This means that your RV is going to start pushing against your LV.
Your interventricular septum is the fancy name we call the tissue that separates your RV from your LV. Under normal circumstances, that septum shifts towards your RV, making your RV crescent shaped from above (e.g. if you were looking at a cross-slice of your ventricles).
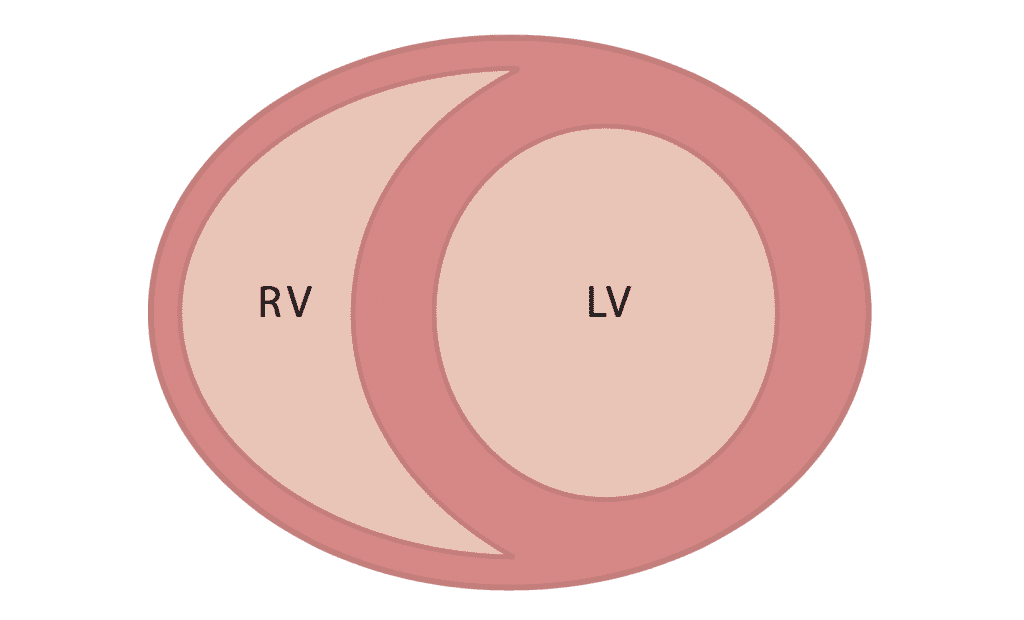
Now back to our PE patient – as that pressure builds up in the RV, that septum is going to start bowing (leaning) the other way, crushing the LV.

As that RV continues to deal with higher and higher pressure, it will eventually be unable to squeeze against these high pressures AND the septal bowing may become so severe that it compresses your left ventricle stopping cardiac output.
This is why a PE can become so dangerous. The upstream effects that that clot can cause can be disastrous.
And that’s it for today’s discussion. Not leaving on the happiest note, but hope going through the anatomy and pathophys today was helpful before moving into more specifics like diagnosis, signs and symptoms, and of course – treatment.
Keep cool out there!

One thought on “Venous thromboembolism (VTE) Part☝️: Introduction”