Now that we’ve solidified the basics of valves – why we have ’em, how they work, all the squirrely stuff that can go wrong with them – let’s talk about how we actually can treat these patients.
We’re going to be reviewing treatment of these conditions prior to surgery/replacement and then review what therapies these patients should start on after they get their bright new shiny valves.
Now, the therapies below for our “pre” valve replacements are not a fix – they are merely bandages while you figure out when your patient can go for replacements.
This talk today will only focus on surgical valve replacement – part 3 will focus on other methods of valve replacement (e.g. TAVRs).
Understanding the pathophys of what’s going on with these valves will be very very important! So if you haven’t plz read part 1 first because I will only be doing a basic recap here.
“Treating” Valvular Disease Prior to Surgery
Aortic Stenosis
OK – so in aortic stenosis (AS), we have this really crusty, calcified, narrowed aortic valve.
Keep in mind that the aortic valve is our gateway between the left ventricle and the aorta – it’s the last stop in the heart before blood is shot out to the rest of the body.

Managing blood pressure in these patients is going to be key prior to them getting their valves replaced.
Afterall, put yourself in the shoes of your left ventricle.
In aortic stenosis, that LV is already struggling to get blood out and keep forward flow because it is quite literally trying to push all this blood through a teeny tiny cocktail straw (think about how your cheeks feel after blowing through a slurpee straw versus a cocktail straw for a long period of time). It’s going to create chronic high pressures in the LV (and thus over time hypertrophy and heart failure).
The last thing we want to do to that poor LV is make it even harder to get forward flow by having your patient run grossly hypertensive.
With high blood pressures, that huge afterload that the LV already has to pump against is just going to get even worse. The rule of thumb in these patients is that we’d love to avoid gross hypertension because of this.
But….it gets complicated *bum bum bum*. Let’s talk about why.
Quiz question/check your memory: What are the two determinants of blood pressure in the body? AKA what is the formula for blood pressure?
*insert brain storming here*
If you don’t remember – totally cool – but I’d recommend a refresher (check out the hemodynamics OG post).
Blood pressure is determined by both 1) blood volume and 2) squeeze of vessels.
Our blood volume is represented as cardiac output (CO) – aka the amount of blood your body gets per unit of time. The squeeze of vessels is known as systemic vascular resistance, or SVR.

Let’s say you gave your patient with severe AS a fast acting and potent antihypertensive. Could be something like IR nifedipine or a push of an IV antihypertensive agent (IV hydral I’m looking at you 🙄 🙄 🙄 🙄 🙄 🙄 )
Now, just like all of us humans, your body doesn’t LOVE change, right? It likes to keep homeostasis; it loves keeping up appearances and keeping everything stable up in there.
So you give an IV anti-hypertensive that works on vasodilating/relaxing the vessels – what factor is going to change in our BP equation?
SVR! right?
So then SVR is going to drop it like it’s hot and in order to avoid actual hypotension, what is your body going to do in response?

It’s going to have to figure out a way to increase cardiac output, right?
Now normally, the body would undergo reflex tachycardia to help compensate, get cardiac output up and preserve blood pressure.

Keep in mind that cardiac output is a measure of the amount of blood your body is getting per unit of time, aka stroke volume multiplied by heart rate.

In severe aortic stenosis, though, your aortic valve opening is literally so restricted and small, that reflex tachycardia ain’t going to increase the amount of blood leaving your heart – in other words, given the severity of the AS, your cardiac output will remain fairly fixed in the setting of a potent decrease in SVR.
What this leads to is a potentially life-threatening case of hypotension – since your body cannot compensate like it would normally do.
Because of this, we really, really, really want to avoid anything that can mess with SVR too rapidly and potently, like IV boluses of antihypertensives or fast acting oral agents like IR nifedipine.
The rule of thumb in aortic stenosis is: if we’d have to pick, we’d rather have these patients run a little high than risk dropping them too low. And that reason all boils down back to pathophysiology.
Mitral Stenosis
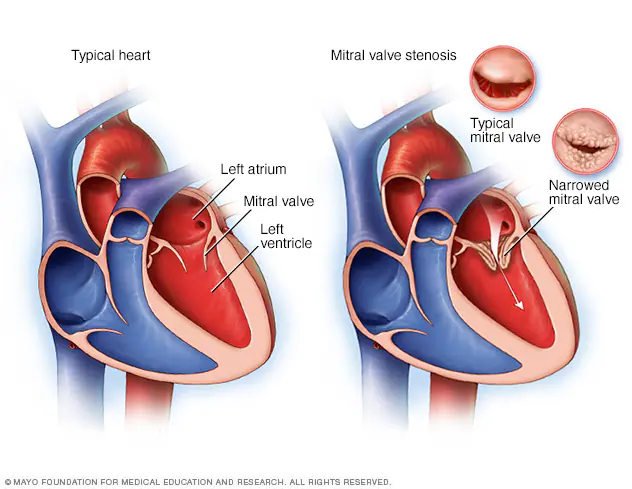
Alright next up to bat are patients with mitral stenosis, aka a really narrowed mitral valve. To reorient ourselves, the mitral valve is the valve that sits between the left atrium and the left ventricle.
Let’s keep in mind how it feels to be the mitral valve. Very Gen Z of me I know (kidding). But seriously.
If you were standing on the mitral valve, what are you experiencing? What kind of pressures are you seeing?
If you remember from our basic hemodynamics and coronary anatomy posts, you might recall that amount of pressure the mitral valve sees is….. pretty….minimal, at least compared to the pressure that the aortic valve experiences.
Sure, there’s a lil bit of an atrial kick, but it’s minimal compared to the crazy crushing squeezing force of the LV.
The majority of blood flow movement through the atrioventricular valves (aka both the tricuspid and the bicuspid valves) is passive. What I mean by this is that the mitral valve will open – the left atrium will do a little *ehhhhh*, and then most of the blood will just flow through during that period of diastole.
Why did we review this? It’s because the “treatment” for mitral stenosis patients draws exactly on this concept.
Again – tightened tiny narrowed mitral valve, mostly passive blood flow – what can we do to potentially increase the amount of blood that flows through the mitral valve?
Any ideas?
Two words: beta blockers.
In case you didn’t guess beta blockers – I want you to think about it – why do you think it would make sense to use beta blockers in the setting of mitral stenosis?
What do beta blockers do to our hemodynamics?
By decreasing the ability of norepinephrine and epinephrine to bind to the beta-1 receptor, we slow down heart rate.
If you slow down heart rate, you are effectively decreasing the amount of ventricular contractions per unit of time (e.g. instead of 100 beats per minute, you’re down at 60 beats per minute).
If we are decreasing the amount of time spent in systole, then we are….increasing the amount of time spent in diastole.
And by increasing the amount of time spent in diastole, or ventricular relaxation – you guessed it – we are increasing the amount of time that the blood has to passively go through that stenotic mitral valve. And thus we help increase the amount of blood that flows forward into that LV.
Aortic Regurgitation
In aortic regurgitation, the issue is that we have a leaky aortic valve and instead of getting all that blood out in forward flow, a portion of it will leak right back into the left ventricle during systole.
In order to promote forward flow, we want it to be as favorable as possible for blood to want to go into the aorta as possible, right? We want to make the forward route into the aorta enticing, make it as appealing as we can.
How can we nudge the blood to try to keep forward flow?
By decreasing the intra-aortic pressure (aka the pressure within the aorta), or afterload, we are making it as easy as possible for that blood to want to continue with forward flow.
And so in aortic regurg, we can opt to use vasodilator therapy to help reduce some of that hemodynamic burden in some patients, especially vasodilators that target the arteries and cause decreased afterload.
This helps by enhancing forward flow – but there’s not really good data that this actually changes outcomes.
Because of this, you only really see vasodilators recommended in severe aortic insufficiency and only long-term in patients who are poor candidates for replacement or short term to help improve the hemodynamic profile prior to replacement in those with severe LV dysfunction or with heart failure symptoms.
Mitral Regurgitation
Whenever you are thinking about adding on some meds to help out patients with mitral regurg, it’s important to first figure out what kind of mitral regurg they have.
For example – if they are mitral regurg due to a really thinned walled, structurally damaged dilated left atria, you can consider using drugs that reduce preload to help with the extent of the dilation.
If patients have both mitral regurg and classic LV dysfunction – they become candidates of GDMT for HFrEF. Unfortunately, for patients with ischemic mitral regurg, there’s not any widely accepted recs to help medically manage these patients. Like any of the other types of valvular disease, once your patient starts getting symptoms, you really should start considering replacement as a definitive treatment option.
When to consider replacement.
This is out of my wheelhouse as a PharmD (s/o to the interdisciplinary team!), but in a nutshell, there are certain things that providers want to assess before making the decision to replace a valve. We don’t want to put the patient through a ton of hassle with getting their valve removed and replaced if it’s not clinically significant. As a quick overview, there’s a few core tests that are generally used to assess these patients.
The standard diagnostic test that is generally used to evaluate these patients is the transthoracic echocardiogram (TTE).
Echos are utilized to physically see the structure and function of the heart – the chambers, the valves, the size of the aorta, etc.
Using fancy tools with ECHO (like Doppler ECHO), the team can determine the hemodynamics around the valve noninvasively.
For stenosis, measurements like maximum velocity, mean gradient, and valve area are often taken.
For regurg, regurg orific area, volume and fraction is checked.
Depending on the severity of these measurements along with patient presentation, the decision whether or not to repair or replace will be made by the interdisciplinary team.
Definitive Treatments: Repair or Replacement!
We’ve come to the final part of our discussion on valvular disease in the heart – replacement.
For many patients, this will be their best bet at long term durable outcomes.
The landscape of valve replacement has really, really changed over the past few decades. It’s really incredible to see how far we’ve come in such a short period of time.
The History of Heart Valve Replacement
Let’s jump back into the wayback machine and head to the 1950s – really not that long ago if you think about it.
The first real kid on the block was Charles Hufnagel – a physician and a surgeon from Georgetown who is generally credited with making the first ever prosthetic heart valve.
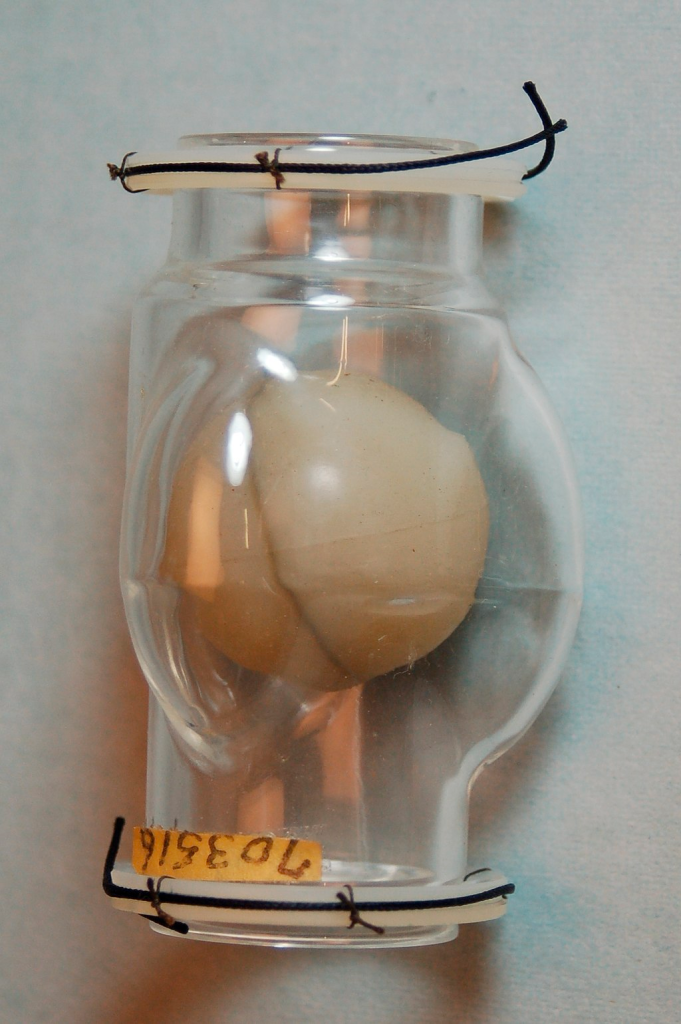
His technique was different than what we are used to today – he created an extra valve – known as an aortic “assist” valve in the descending aorta of a patient with aortic regurgitation out of plastic. The purpose of the valve was not to replace the faulty leaky aortic valve of the patient, but rather to ensure forward flow at the point after it, preventing backflow back in the ascending aorta and back into the heart. The valve was about 1.5 inches, made of plastic, and consisted of a free moving plastic “pea” inside of a tube. That pea would be dislodged by pulsating blood with each heartbeat, closing during the period of diastole.
Dr. Hufnagel performed the first ever successful implantation of an acrylic ball valve in the descending aorta in a 30 year old female with severe aortic regurg.

The next big pioneers included Dwight Harden, in 1960s, who invented and implanted a new type of design – known as the ball and cage heart valves (known as the Harken-Soroff valve), along with another type of ball and cage valve created by Dr.s Starr and Edwards – aptly known as the Starr-Edwards Valve.
Believe it or not, the design for these valves came from the idea of old bottle stoppers. These valves were put into the more standard position we are familiar with these days – aka in the annulus of the valve itself.
The first ever successful mitral valve replacement was performed by Starr and Edwards and their original manuscript can easily be accessed online for free.
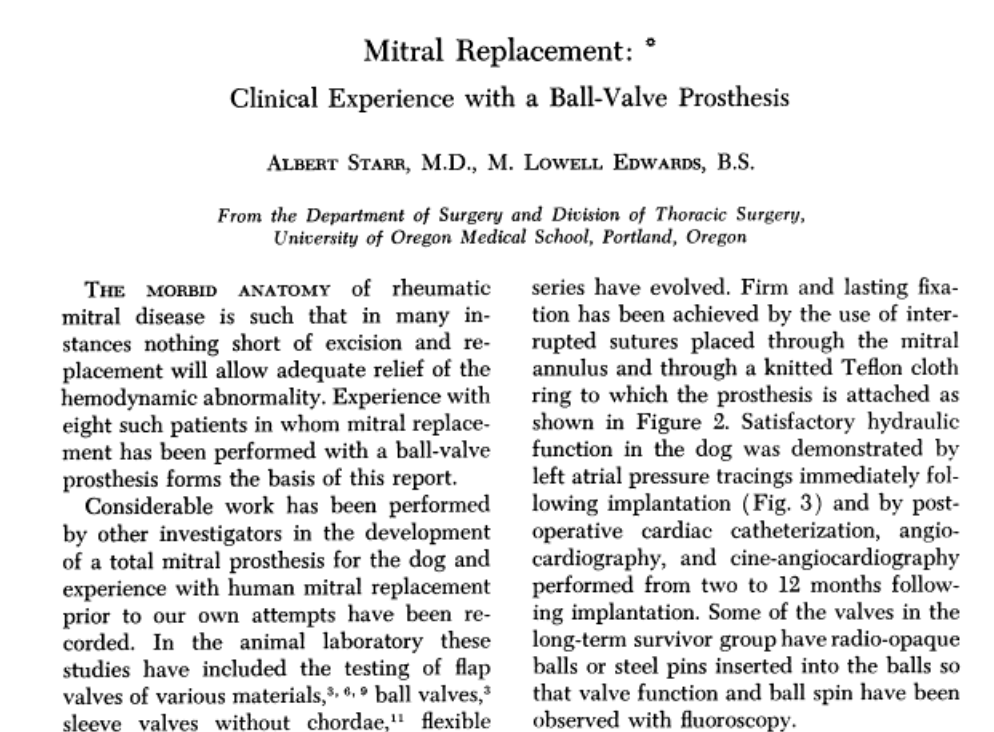

Source: reddit.

Another interesting piece of history to note is Dr. Harden – the surgeon above – started his career in the 40s by figuring out a way to treat mitral stenosis by quite LITERALLY cutting a small hole in the heart, blindly going in, and sticking his finger into the heart and literally opening up the crusty heart valve with his finger. They called this technique at the time “closed heart surgery”. Unsurprisingly, the majority of patients died in the beginning but as they practiced, the mortality rate decreased over time.
My point is – even just a few decades ago – in the lifetime of many people still living today – we were quite literally poking our fingers into hearts and wiggling our fingers around to treat patients. We have come such a long way, but it’s important to really appreciate and respect the journey that we’ve made in such a relatively short period of time.
These early ways were far from perfect – and it became clear that there was a need for surgeons to actually gain access to the inside of the heart and work from within – but they quickly ran into a problem.
If they kept circulation running, your patient would bleed to death if you tried to open up their hearts – but if you stopped circulation temporarily, you only bought yourself about 4 minutes to work before the patient started undergoing brain damage. IDK about you, but I can barely make a cup of coffee in that amount of time, let alone start and finish heart surgery.
It wasn’t until 1953 when the first heart-lung machine was introduced – by bypassing the blood from going into the heart and lungs and artificially oxygenating the blood, this made the idea of open heart surgery a reality for the first time in history. The first ever surgery was to repair an ASD (atrial septal defect) in an 18 year patient who lived over 30 years afterwards.
Before we continue on to talk about the evolution of these early valves – let’s talk about the implications that having these valves placed might cause.
If you think about it,
The ideal heart valve would be durable, physiologic, recognized as the body’s own, and have a very sleek and favorable hemodynamic profile that would mimic our natural valves.
Obviously the ball and caged valves…….are far from this. Like seriously – anything BUT sleek.
What do you think a consequence of having this foreign object valve placed into your heart?
Besides common things like bleeding during the operation or the risk of infection that comes with any large procedure, one of the biggest issues we face with artificial valves is thrombosis.
If you need a refresher on thrombosis and the clotting cascade, check out that post under archives. When an existing valve is replaced, the patient’s coagulation system will be activated on both sides – both the intrinsic and extrinsic clotting cascade.
The damage and irritation to the tissue will active the extrinsic clotting cascade (aka tissue factor will be released and the process will start up leading to fibrin formation) – and the presence of this new foreign object (the valve itself) – will activate the intrinsic clotting cascade.
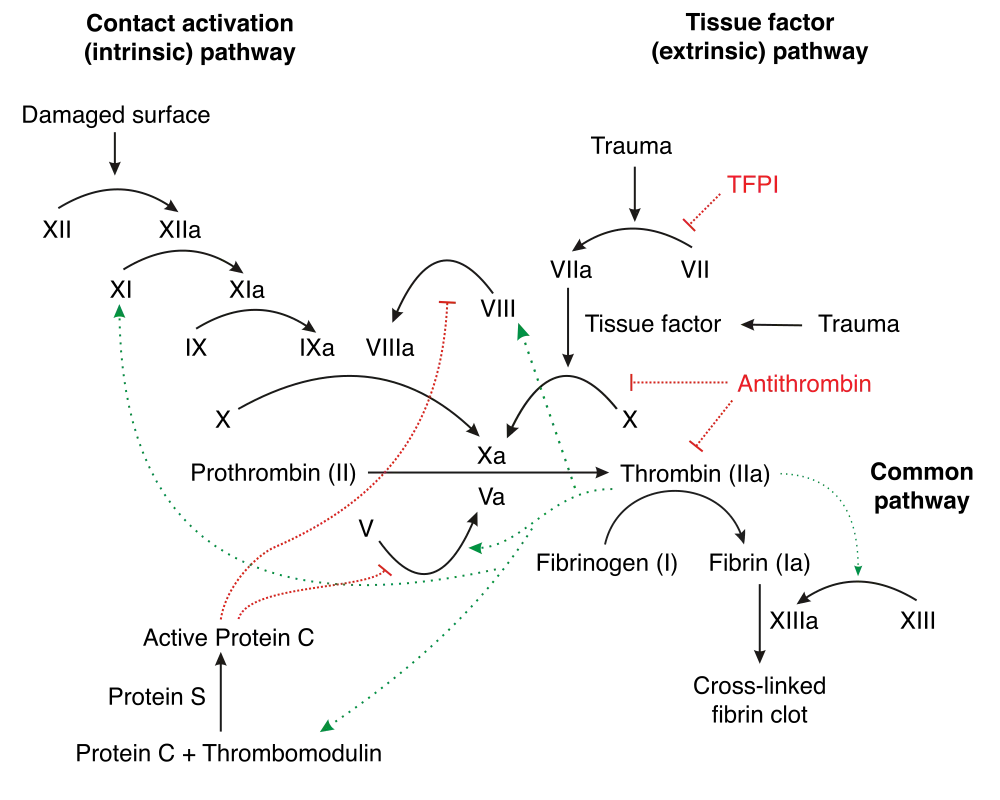
Thrombosis is therefore a big complication of getting a heart valve. Keep this in mind going forward.
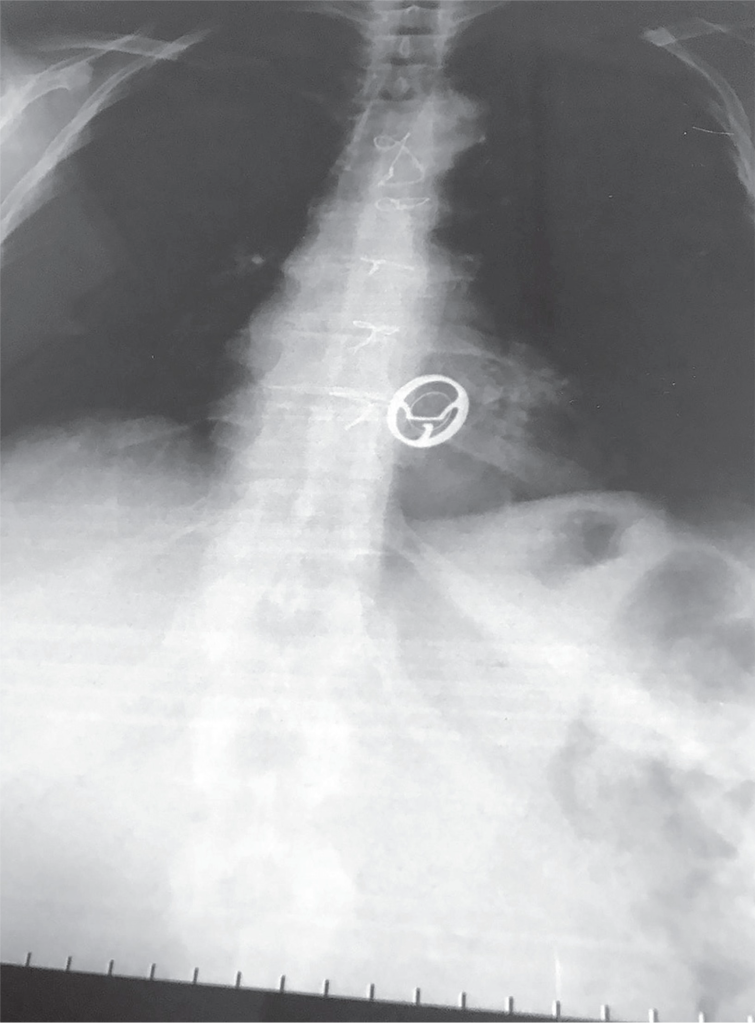
Another interesting nuance about the ball and cage valves is noise – these bad boys were pretty loud as they moved back and forth.
If you are lucky enough to meet a patient that has one of these old generation valves (and yes, they are still around), you should be able to hear the ticking if you are silent next to them.
I had a patient with a Starr-Edwards Ball and Cage valve once that would joke with me that their least favorite part of the valve was that it messed up their poker game, since their heart rate would change when they got a really, really good hand. Talk about giving away your hand.
It eventually became obvious that these patients needed something to prevent thrombosis of their valves and warfarin became the standard of care. Why warfarin?
Well, warfarin was pretty much our only oral anticoagulant at that time.
With the large surface area and turbulent flows associated with the ball and cage valves, the hunt for a more streamlined, more physiologic valve was on.
Before you knew it, a new generation of valve was developed, one with a leaflet that would rotate open and close with each beat – also known as a “tilting disc” valve.
A team consisting of both an engineer and a heart surgeon (Donald Shiley and Viking Björk, respectively) came together to create the first successful-tilting disc valve – known as the Björk-Shiley valve. The valve got its feet off the ground in 1971 and was used to replace both aortic and mitral valves.

These valves made of a mixture of metals and carbon were very popular and widely used in the 1970s – however, in a few years, it became apparent that these valves had some durability issues in the long term, and could shed microscopic metal fragments. Woof.
Starting in 1979, the design was changed to help speed manufacturing and to make flow more physiologic – however, as a result, a weaker structure with more issues arose. These convexo-concave valves could fracture and cause sudden cardiac death.
Because of this, the FDA withdrew approval of the valve in 1986, and a multi-million dollar lawsuit was settled. Some patients still have this valve implanted – the decision and benefit of replacing the valve does not always exceed the risks of another open heart surgery.


The search to improve hemodynamics continued over the next few decades – landmark valves included the St. Jude Medical (SJM) bileaflet mechanical valve in the 1970s. Bileaflet valves allowed for three flow areas through the valve with a more uniform physiologic flow.
The more hemodynamically streamlined, the less turbulent, and therefore the lower the risk of stagnation and therefore thrombosis. Bileaflet valves are still used today.

Bioprosthetic Valves
But what about non-mechanical valves? There is a whole other category of heart valves known as bioprosthetic, or tissue, valves. The history of tissue valves started back in 1962, when Donald Ross performed and created the Ross Procedure, which was used for patients in need of an aortic valve replacement.
The procedure was pretty badass. The Ross procedure involved cutting out a patient’s aortic valve, and replacing it with the patient’s own healthy pulmonic valve. The empty pulmonary valve spot would then be filled by a pulmonic valve from a cadaver.

Why use a patient’s own native pulmonary valve just to replace the old pulmonary valve position with a cadaver valve? Why not just replace the aortic valve with the cadaver valve? Why have the patients go through more cuts and why not just leave the pulmonary valve alone?
Keep in mind that the aortic valve has to be the toughest valve in our heart – it sits right next to the left ventricle and therefore has to tolerate the largest, toughest pressures in the body.
The idea was that a cadaver valve will be flimsy at best to start with, and would likely not be able to tolerate these pressures long term. Therefore, it was thought to use to “next best thing” – the patient’s own native valve that has to tolerate the somewhat high pressures of the right ventricle – aka the pulmonary valve. It’s not perfect, but it’s better than a dead person’s valve I guess.
However, when Ross started out trying to fix aortic valves, the cadaver valves he tried to put in……disintegrated.
In 1962, the first valve replacement from a human cadaver was done by Alfred Gunning with a cadaver valve that was previously freeze-dried. With this technique, Gunning gave some of these freeze-dried valves to Ross, who was then able to replace a valve with the patient recovering well afterwards. Fantastic!
The idea of using bioprosthetic valves – which made sense – was that “our entire physical makeup and body structures represent the end result of millions of years of evolutionary development” and that we would be unable to exactly replicate this through a (wo)man-made mechanical valve.
Because cadavers were difficult to obtain and likely costly, the search also turned to other animals, like pigs or cows. But biologic valves from other sources came with their own slew of issues – the most obvious one being tissue breakdown. Since we’re talking about actual tissue, they had to figure out a way to both sterilize and preserve tissue so it didn’t cause infection or broke down the second you put it in.
They discovered a method of preservation that helps to preserve the valve, prevent rejection, and keep calcification at bay. With these techniques, it was found that the cow (bovine) valve lasted about twice as long as the pig (porcine) valve, making the cow valve the tissue valve of choice.
These tissue valves are generally positioned on a plastic or metal thing stent covered with fabric, or can be stentless and come with a portion of the aortic root really reinforced. See some examples below:

Bioprosthetic versus Mechanical Valves: Who gets what and why?
Once bioprosthetic valves were introduced, there now became an option for patients – prior to their introduction, the only thing that was really available were mechanical valves.
With different choices, came measuring and weighing out pros versus cons.
Thrombosis | Need for Oral Anticoagulation
A common complication of valves in general was the risk of thrombosis. When thinking about tissue valves versus mechanical valves – which do you think would carry a higher risk of thrombosis over time and why?
Think back to the triggers of our coag cascade.
Implanting a new valve, no matter what it’s made of, will initially cause some tissue injury and endothelial damage at that site, triggering the extrinsic coag cascade. However:
Mechanical valves are foreign and made of metals, and so with them comes a big risk of thrombosis. Additionally, the body never will fully accept and endothelialize that valve, and so a portion of it will always remain available to the bloodstream and be a risk factor for thrombosis.
Meanwhile, tissue valves still carry a risk of thrombosis but it is much, much lower. Over the span of a few months, your body will start to endothelialize over that valve and incorporate it into the wall of the heart (in a process very similar to coronary artery stenting – check out the ACS posts if you are confused).
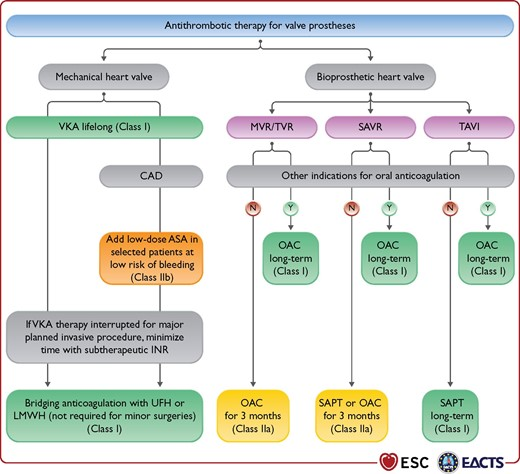
Because of this, patients who receive a mechanical valve immediately buy themselves lifelong anticoagulation. In contrast, patients who receive bioprosthetic valves either do not need OAC at all or may just do a short term course, depending on what valve is replaced (we’ll get to this later).
Because of this, in patients who have high bleeding risk factors, a tissue valve may be better for them.
No matter what type of valve your patient gets – whether bioprosthetic or mechanical – whether in the aortic or mitral position, some antithrombotic therapy will be needed – but lifelong OAC is really reserved especially for those with mechanical valves.
Durability
Bioprosthetic valves versus mechanical valves also have very different “life spans”. Mechanical valves are ….. mechanical!, therefore once you get one, it should really last lifelong (unless you encounter other complications).
However, once a tissue valve is put in, you really only get a good 15-20 years out of that valve if you are lucky, and may be even less than that.
Who gets what:
This is a generalizability and not true for all patients, but usually the really old patients or really young patients are a little bit more “clear cut”.
In our very old patients, we will likely opt to do a tissue valve. This way, they won’t need to be put on long term OAC (and keep in mind the elderly tend to have increased risks of bleeding as well as well as falls) and chances are, that tissue valve will last them the remainder of their lifespan.
In our very young patients, we often will STILL opt to do a tissue valve. Why? Again, a generalizability, but often younger patients tend to be more active, involved in more “dangerous” activities (like climbing up ladders or playing football).
Because of this, we wouldn’t necessarily love to commit them to LIFELONG oral anticoagulation from the start. By implanting a tissue valve, we give them another 15ish years without committing them to anticoagulation and then the idea is by the time that valve is spent, they will still be well and young and healthy enough to get another sternotomy (if need be).
The middle aged patients may often be the hardest to decide on. Other factors to consider in these selections are patient occupation (e.g. sits at a desk all day versus…..a lumberjack), compliance (because if they don’t want to take OAC, that valve has a high risk of clotting up), etc.
The Operation Itself
Not a lot to say on this (clearly not in my wheelhouse as a clinical PharmD), but hopefully it makes sense that if a surgeon is replacing a valve, your patient 110% has to be put on cardiopulmonary bypass. This should make sense, since the surgeon literally has to cut directly into the heart to access the valve. If blood was still flowing through the heart – well, your patient would die on the table and bleed out pretty quick. And so they bypass the heart and the lungs, and stop the heart.
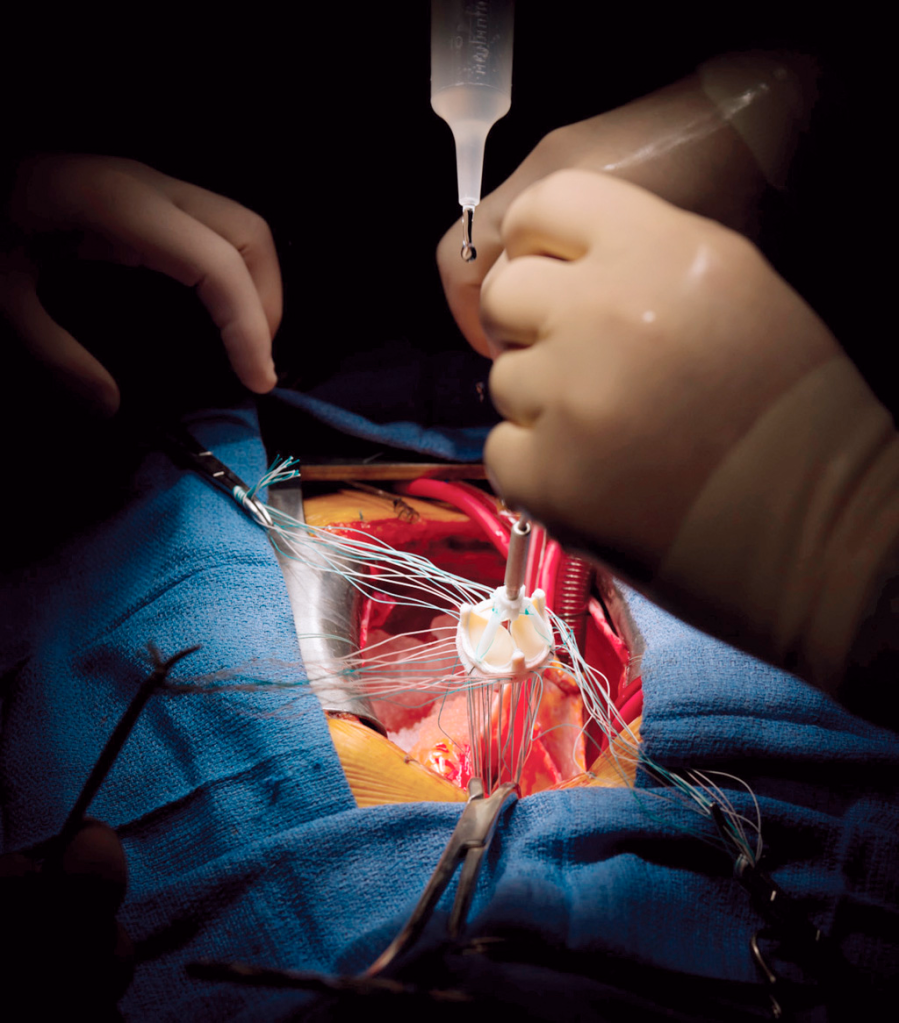
The surgery is also super interesting – if you ever have a chance to observe one, I highly highly recommend it. I have a ton of respect for CTS surgeons in general and especially considering the amount of dexterity they need to sew these valves in.
CTS surgeons will basically take out the existing valve, start suturing up the new replacement valve outside of the chest cavity before slowly sliding it into place and finishing up the sutures. Like can we appreciate the amount of stitches and handiwork these people have?! They must be really good at stitchwork/embroidery too if they put their minds to it.
Pharmacotherapy After Surgical Valve Replacement
Alright my friends. Next up we have to talk antithrombotic regimens. We already know that mechanical valves have a higher risk of thrombosis with them, and with that – a lifelong ticket to oral anticoagulation. But does the degree of anticoagulation differ based on which valve we’re replacing?
And what about bioprosthetic valves? You’re still cutting into the valve area and leaving in a semi-foreign object (afterall, it’s usually made from a cow) – these should theoretically activate both the intrinsic and extrinsic coag cascade.
Let’s talk through the two most common valve replacement positions: the aortic valve and the mitral (bicuspid) valve.
Try to think your way through this: which valve position do you think has a higher risk of thrombosis?
Need a hint? First think about the factors that influence thrombosis and clot formation in general.
The big three that we usually think about are: stasis, hypercoagulability, and injury.
In theory, both positions – whether the mitral valve or aortic valve – should undergo a similar degree of tissue injury during the procedure. No matter what the position, the surgeon still needs to cut out your defective old valve and suture in a new valve.
Now what about the amount of stasis these valves go through?
We’re going to Magic School Bus Miss Frizzle this.
Once again – imagine yourself hanging onto that mitral valve in the left atrium. The mitral valve sits between the left atrium and the left ventricle.

What kind of pressures and blood flow are you experiencing? In order to think about this, keep in mind what normal heart function looks like. If you remember from our core talks, you’ll remember that – sure there’s a lil bit of an atrial kick as the atria depolarize, but the majority of blood flow from the atria to the ventricles is passive – in other words, the blood moves on its own simply due to the AV valves being open.
Honestly, thank god this is the case because if we really relied on atrial contraction for perfusion, patients in AF would be in a lot of trouble.
Anyway, on that mitral valve – you’ll likely not experience super high, fast pressures and blood flow movement. At least relatively speaking.
Now let’s Miss Frizzle the aortic valve up in here. Imagine you are sitting on the aortic valve.
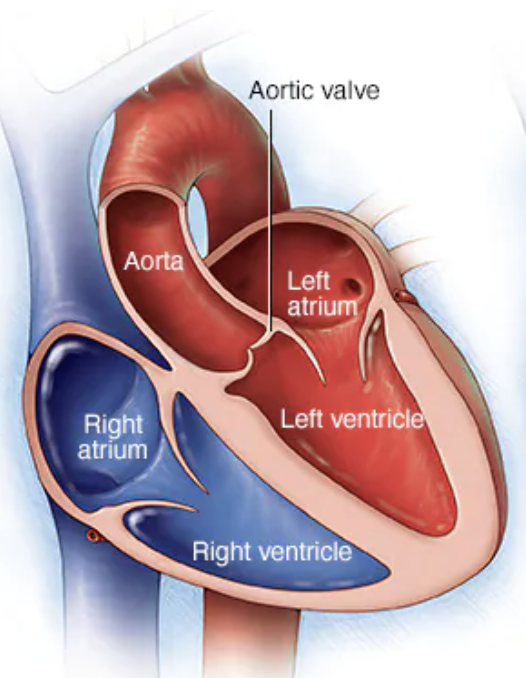
Keep in mind the aortic valve is aptly named since it sits between the LV and the aorta. What kind of pressures is the aortic valve experiencing compared to the mitral valve? High? Low? The same?
Waaaaaaaaay higher. The LV is the workhorse of the heart – the Dwayne the Rock Johnson of those chambers. It is meant to generate high contraction and high pressures.
Because of this, valves in the aortic position are less likely to form clots compared to those in the mitral position. Afterall, the aortic valve is seeing higher pressure/flows and therefore the blood there experiences less stasis. Less stasis = less thrombotic risk.
And so – keep this in mind when we discuss antithrombotic agents post surgical valve replacement.
Antithrombotic Therapy s/p Surgical Mechanical Valve Replacement
Let’s start with mechanical valves. As we talked about above, these patients need oral anticoagulation lifelong because that valve never completely endothelializes and becomes accepted as our own.
We know the only main oral anticoagulant we had was warfarin. And for years we have nothing else we could give orally. Untilllllll…..
In the 2010s, we finally had the introduction of the direct oral anticoagulants – the DOACs.
The DOACs were a very exciting time for cardiology history – after all, for the first time we had medications that had lower risk of intracranial hemorrhage, are taken orally, and didn’t need frequent INR monitoring.
But in order to really see if they are efficacious in this patients population – we have to study them.
Cue the REALIGN trial.
The REALIGN trial was conducted in 2013 and sought to answer the question – can we use DOACs instead of warfarin in patients with mechanical valves?
And so this 2013 trial looked at dabigatran versus warfarin in patients with mechanical heart valves.
Aaaaaaaaaaaaaaaaaannnnnnnnnnnnnnndddddd….
The trial had to be stopped early due to an excess of both thromboembolic AND bleeding events in patients in the dabigatran arm. 😭😭😭😭😭😭😭😭😭😭
A sad day for medicine.
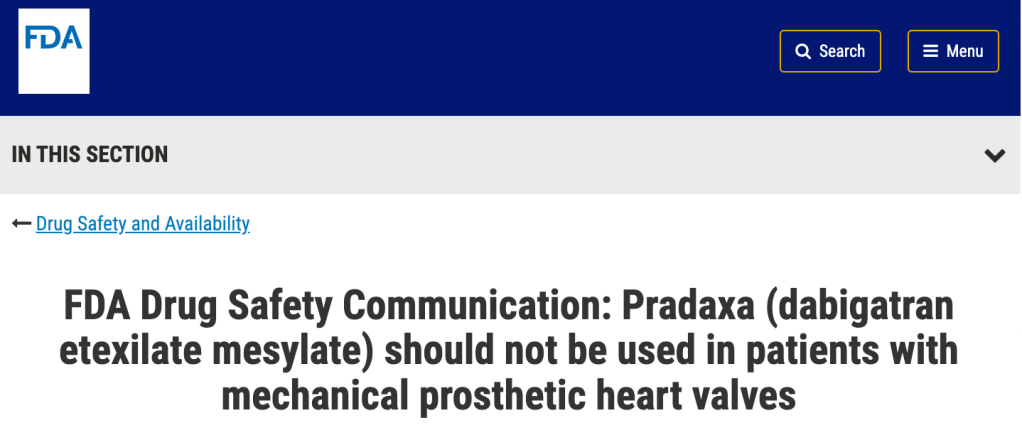
Because of this, if you check out any valvular disease guideline, you’ll see that there is a class III (harm) recommendation that you cannot and should not use dabigatran in patients with heart valves.
What about the other DOACs you might ask? Well, for one- I’m not sure I would be the one brave enough to retrial this with another DOAC in this same patient population.
In a few minutes, we’ll get to a more recent trial that studied another DOAC in patients with a very specific types of heart valve and whether the decision to use DOACs in patients with mechanical heart valves has changed.
But for now – for the most part – warfarin it is. She ain’t going anywhere anytime soon.
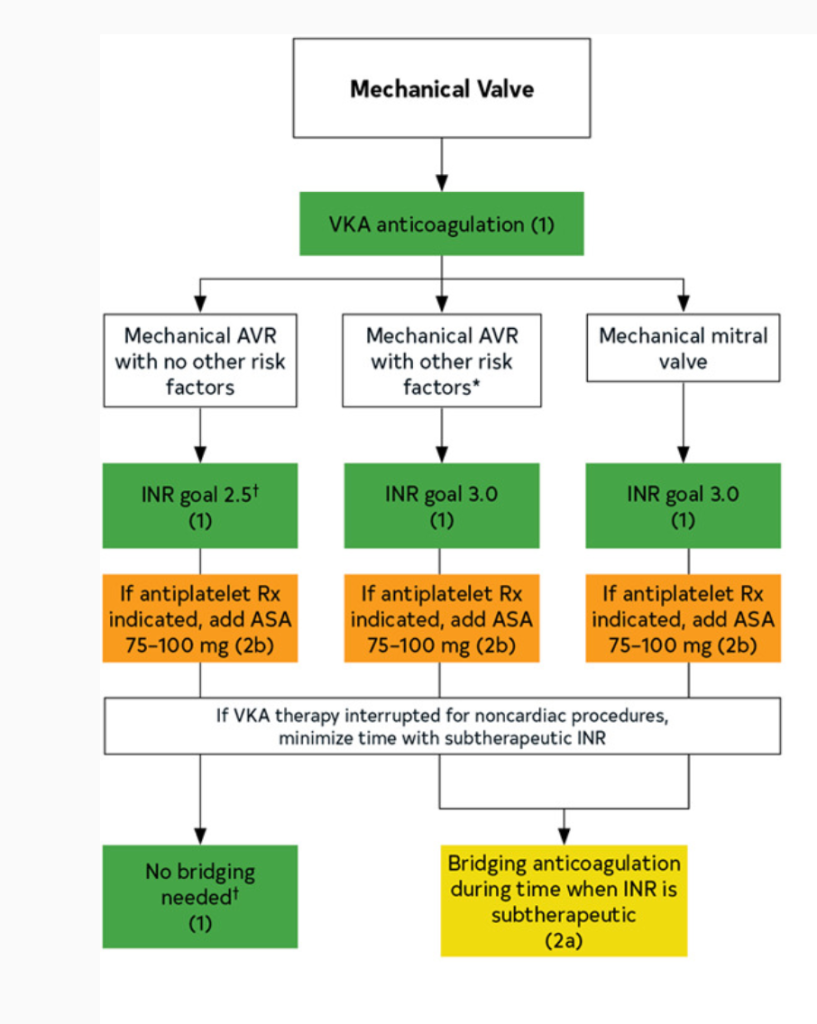
However, the INR goal is going to depend on where the valve location is. Since the mitral valve is more thrombotic of a position than the aortic valve for reasons listed above, theI INR goal is higher in mitral mechanical valves (in other words, we thin out these patients’ blood MORE).
In patients with mechanical heart valves, all need lifelong warfarin. However:
Aortic mechanical valve (most types): warfarin with INR goal 2-3 indefinitely
Mitral mechanical valve: warfarin with INR goal 2.5-3.5 indefinitely
This is the “standard” treatment for most patients.
Special Populations:
If you look at the 2020 American disease guidelines, you will notice that a higher INR goal can be considered if a patient has both a mechanical heart valve and other risk factors for thrombosis.
These all include patients who are more likely to form clots at baseline, such as patients that also have atrial fibrillation, other hypercoagulable states, really bad systolic heart failure (remember – low squeeze means higher risk of clot!), or in patients that have older valves (like that ol’ hunk ball and cage ones – since those are old and have such a high surface area, we usually will do 2.5-3.5 for these patients.
Lastly, in select patients, you may opt to add on a baby aspirin in addition to the warfarin therapy above – however, this is really for patients that have another indication for baby aspirin (e.g. hx of ACS, PCI, etc). Since they are already being fully anticoagulated, the decision should be made with care based on your individual patient.
Before we move on to bioprosthetic valve care, there’s one special type of mechanical valve we need to talk about first. It’s known as the “On-X” valve.
Keep in mind the big “con” that comes with mechanical heart valves is the need for full-intensity anticoagulation with warfarin.
So it would be in a company’s best interest to figure out a design of a valve that decreases the rate of thromboembolism and either eliminate the need for OAC (unlikely) or at least lower the “intensity” of warfarin therapy needed.
Cue the On-X valve. (i’m not sponsored i swear (but if anyone wants to pay me hit me up, I’m good 4 it)).
The makers of the On-X valve believed that their special valve had a lower risk of thrombosis when compared to the other available types of mechanical heart valves.
And so they put their money where their mouth was and did a trial to see if patients with this special valve would be able to get away with lower intensity of warfarin anticoagulation.
This was studied in the 2014 PROACT Trial.
And – they found that lower intensity warfarin did not carry a higher risk of thromboembolism, and also had a significantly lower risk of bleeding. WAHOOOOOOOOOOOOO! But wait:
A few key things to note about this trial:
- They only studied patients who received the On-X in the aortic valve position
- All patients were required to be on standard intensity warfarin therapy (e.g. INR 2-3) for the first 3 months after implantation; afterwards, patients were randomized to either standard intensity therapy (keep INR 2-3) or lower intensity warfarin (defined as INR goal of 1.5-2).
- All patients were required to be on baby aspirin (81 mg/day)
Why are these things pertinent?
The first point – that only AVRs were included – makes sense, especially from a harm standpoint. We know AVRs have a lower thrombotic risk than MVRs and so it would make sense the first step to “get your feet wet” to see if lower intensity would be ok would be to study it in the lower thrombotic risk group.
With that being said, in my opinion these results would not be translatable into valves located in the much more thrombotic mitral valve position.
It’s interesting to note that they didn’t lower the intensity of anticoagulation until 3 months in. Any guesses as to why?
It’s likely because the immediate post-op period comes with the highest risk of thrombosis – over those first 3 months, you are letting the sutures heal and allowing that heart to settle. Once this period passes, your risk of thrombosis is lower. It makes sense that the company funding this trial might want to “cover” patients during this acute period with normal intensity so that they didn’t see a large uptick of thromboembolic events in these patients.
Because of this, in practice, we follow what was done with the trial – and drop the intensity on anticoagulation once you are 3 months post procedure.
And lastly – all patients were on baby aspirin in addition to their aspirin – which is not typically done for your standard patient without any other indication for aspirin. Any ideas why they did this? They probably were worried about extra thrombosis in the lower intensity experimental group so by adding aspirin to ALL patients, they could cover some of this risk while not making the experimental group have a higher risk of bleeding (since even the standard intensity warfarin group had baby aspirin on board).
Long story short – in patients that have mechanical On-X AVRs, we follow this trial and do 3 months of standard warfarin therapy plus aspirin followed by lowering the intensity of warfarin 3 months in to 1.5-2 and keep that baby aspirin on board.
What about the mitral position?
We know that the mitral valve position is more thrombotic, so if the AVR On-X fared well, I think a reasonable question is what about the MVR On-X?
They redid this trial in the MVR position (the PROACT Mitral Trial)- and, initial data was promising. However, the paper was retracted due to issues with stats and when it was reprinted, the lower intensity warfarin did not achieve noninferiority versus standard dose warfarin. Bummer. Too good to be true.
But…..the question of DOACs arises in mechanical valves….again…..
Alright so we’re out of luck for the mitral On-X, but we know that patients with the aortic mechanical on-x valve can be safely managed on a lower intensity of anticoagulation with warfarin.
Knowing that these specific type of mechanical aortic valves are less thrombotic than your standard valve…..it makes sense that the idea of DOACS might want to be rechallenged. After all, the 2013 RE-ALIGN trial that made dabigatran contraindicated in mechanical heart valves looked at more thrombogenic valves and included both mitral and aortic positions.
And so they tested apixaban in these special On-X valves in the aortic position.
Cue the PROACT Xa trial.
They controlled for as many thrombogenic factors as they could – they made sure all patients had an On-X valve and only in the aortic position; they made sure patients were not switched to a DOAC until at least 3 months post implantation. They had a primary efficacy endpoint of valve thrombosis or valve related thromboembolism.
And.
The.
Trial.
Had.
To.
Be.
Stopped.
Early.
😭😭😭😭😭😭😭😭😭😭😭😭😭😭😭😭😭😭😭😭
After 863 patients were enrolled, they had to stop the trial early due to an excess risk of thromboembolism with apixaban, and this is even with 94% of patients also taking aspirin.
In summary, it sounds like DOACs are not going to be an option any time soon for the thrombosis prophylaxis for mechanical heart valves. The PROACT-Xa trial really further cemented this idea.
Antithrombotic Agents s/p surgically placed bioprosthetic valves
Alright! We finished up with the mechanical valves, now let’s talk about what happens to patients after they get either a mitral or aortic bioprosthetic valve placed surgically.
We already discussed how bioprosthetic valves are a lot less thrombogenic. This is because they are more similar to our native tissue and within the first 3 months after implantation, most of that valve gets endothelialized over and accepted as our own.
Bioprosthetic Aortic Valve Replacements
In the aortic valve position – with high flow and high pressures – your risk of thrombosis is fairly low. Because of this, patients who get a bioprosthetic aortic valve only need to be managed with baby aspirin lifelong. That’s enough to cover them from clotting off on this new tissue valve.
The mitral position is a little more hairy – after all it is seeing lower pressures, slower flow. Because of this, some extra coverage is needed during those first 3 months while the bioprosthetic valve settles into its new home in the mitral valve position.
In general, for patients who end up getting a surgically-implanted bioprosthetic (tissue) mitral valve, because of the higher risk of thrombosis, warfarin is given but only for the first three months. This should make sense – we’re going to help support that valve as it goes through the process of endothelialization – after that, the risk of thrombosis is greatly reduced. After that 3 month mark, we will generally drop the warfarin and transition to just a lifelong baby aspirin 81 mg.
Alright. That was a lot today. Phew. Thanks for hanging in.
Next post will focus all about a newish spiffy technique known as TAVR. It involves valve replacement without your typical cardiothoracic surgery techniques (all done via catheter).
See you then!